 Defense mechanisms are often used in the precontemplation or contemplation phases to avoid acknowledging the problem or making behavioral changes.
Defense mechanisms are often used in the precontemplation or contemplation phases to avoid acknowledging the problem or making behavioral changes.
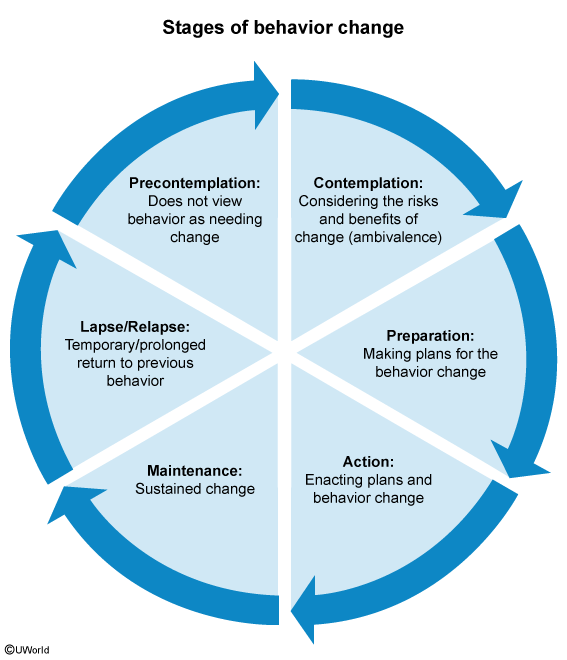
- Stages of Change
- Precontemplation
- Description: Patient does not recognize the problem and has no intention of changing behavior in the near future (< 6 months).
- Key Feature: Denial or ignorance of the consequences. “I don’t have a problem.”
- Contemplation
- Description: Patient acknowledges the problem and is considering change within the next 6 months but is ambivalent t .
- Key Feature: Weighing pros and cons. “I know smoking is bad, but it relaxes me.”
- Preparation
- Description: Patient intends to take action in the immediate future (< 1 month) and has taken some small steps toward behavior change.
- Key Feature: Making plans (e.g., buying nicotine patches, signing up for a gym).
- Action
- Description: Patient has actively modified the behavior.
- Key Feature: Overt lifestyle changes have occurred but have lasted < 6 months.
- Maintenance
- Description: Patient has sustained the behavior change for > 6 months.
- Key Feature: Focus shifts to preventing relapse.
- Relapse
- Description: Return to previous problem behavior.
- Key Feature: Accepted as a normal part of the cycle; not a failure. Patient re-enters the cycle (usually at Contemplation or Preparation).
- Precontemplation
- Physician Management Strategies
- Precontemplation:
- Do not argue or lecture.
- Build rapport and encourage re-evaluation.
- Ask permission to discuss the issue next visit.
- Contemplation:
- Elicit the patient’s perspective on pros/cons (Motivational Interviewing).
- Emphasize benefits of change.
- Preparation:
- Assist in developing a concrete plan (e.g., set a quit date).
- Discuss potential barriers and solutions.
- Action:
- Provide positive reinforcement and encouragement.
- Discuss relapse prevention techniques.
- Maintenance:
- Continue monitoring and support.
- Reinforce internal rewards.
- Relapse:
- Reassess motivation and barriers.
- Encourage the patient to try again; frame as a learning opportunity.
- Precontemplation: