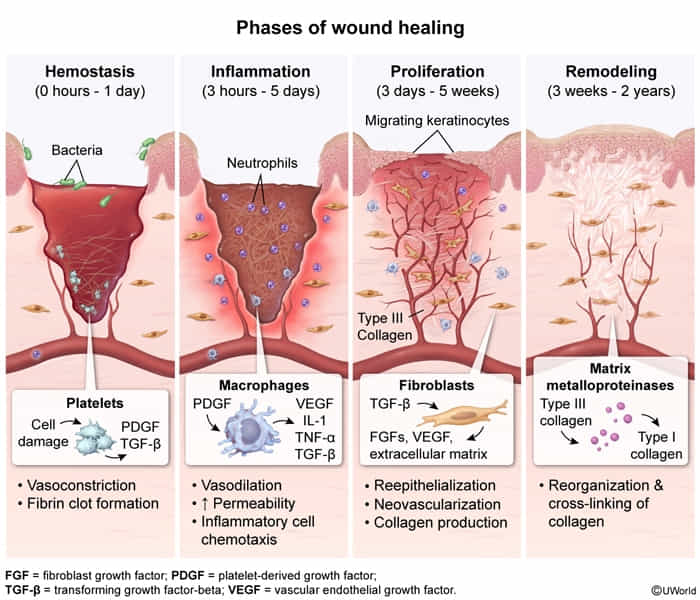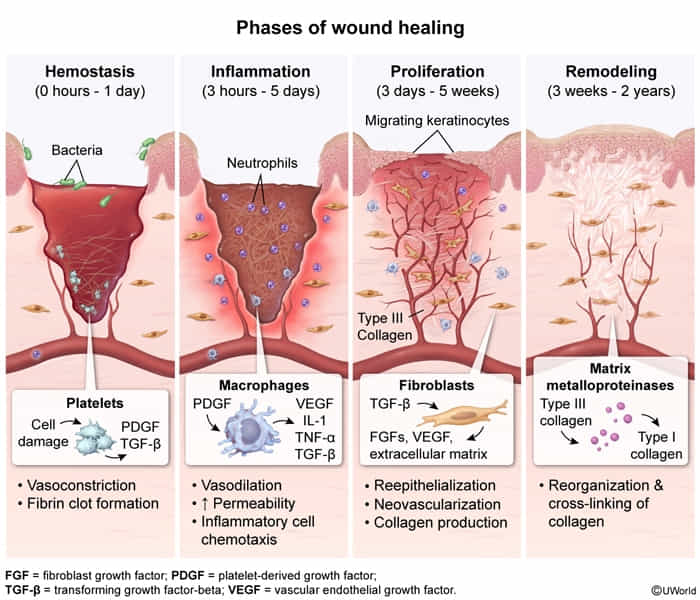
- Timeline & Phases
- 1. Inflammatory (Days 0–3): Platelets (clot) → Neutrophils (clear debris) → Macrophages (Day 2–3; Key regulatory cell).
- 2. Proliferative (Day 3–Weeks): Granulation tissue (Type III Collagen + Angiogenesis). Myofibroblasts cause wound contraction.
- 3. Remodeling (1 Wk–Months): Type III replaced by Type I Collagen (stronger). Mediated by MMPs (requires Zinc). Max tensile strength = 80% (can never reach the original strength of unaffected skin t ).
- Collagen Switching
- Type III: Granulation tissue, embryonic tissue, pliable.
- Type I: Mature scar, bone, tendon, strong.
- Hypertrophic Scar vs. Keloid
- Hypertrophic: Confined to wound borders; parallel collagen; may regress.
- Keloid: Extends beyond borders; disorganized collagen; high recurrence; ↑ in darker skin types.
- Nutrient Deficiencies & Pathophysiology
- Vitamin C: Impaired hydroxylation (weak collagen).
- Copper: Impaired cross-linking (Lysyl oxidase).
- Zinc: Impaired remodeling (MMPs).
- Key Growth Factors
- TGF-β: Major stimulator of fibrosis/collagen.
- Vascular endothelial growth factor (VEGF)/Fibroblast growth factor (FGF): Angiogenesis.
- PDGF: Smooth muscle/fibroblast migration.