Epidemiology
Etiology
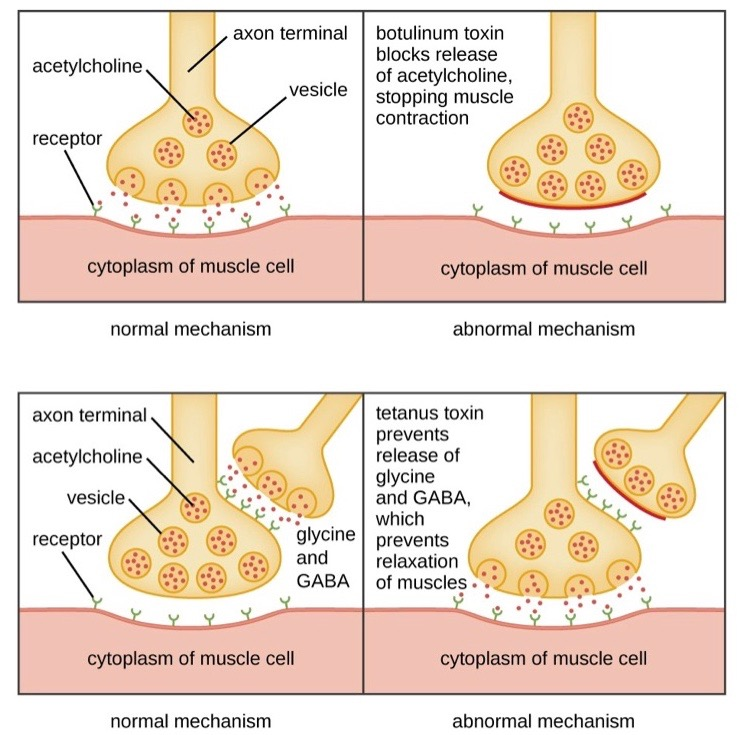
Pathophysiology
- Tetanospasmin: reaches the CNS through retrograde axonal transport
- Toxin binds to receptors of peripheral nerves and is then transported to interneurons (Renshaw cells) in the CNS via vesicles.
- Acts as protease that cleaves synaptobrevin, a SNARE protein → prevention of inhibitory neurotransmitters (i.e., GABA and glycine) release from Renshaw cells in the spinal cord → uninhibited activation of alpha motor neurons → muscle spasms, rigidity, and autonomic instability
- Tetanolysin: causes hemolysis and has cardiotoxic effects
Tetanus vs botulism
Both work on SNARE proteins
Clinical features
- Incubation period: Days to weeks.
- Presents with a descending pattern of muscle rigidity.
- Early signs:
- Trismus (lockjaw): Spasm of masseter muscles.
- Risus sardonicus: “Sardonic smile” from facial muscle spasm.
- Later signs:
- Opisthotonos: Arching of the back due to severe extensor muscle spasm.
- Painful, generalized muscle spasms, often triggered by minor stimuli (noise, light).
- Autonomic instability: Tachycardia, hypertension, sweating.
- Pt remains conscious throughout.
Diagnostics
Treatment
- Immediately manage life-threatening and severe symptoms.
- Administer passive immunization, e.g., human tetanus immunoglobulin (HTIG), as soon as possible.
- Manage acute wounds, e.g., wound irrigation and debridement
- Initiate antibiotics, preferably PO metronidazole.
- Begin active immunization with the tetanus vaccine once the patient is improving.
- Prevention
- Prevention of neonatal tetanus is achieved primarily by vaccination of the mother during pregnancy with an inactivated tetanus toxin (tetanus toxoid) as part of the tetanus-diptheria (Td) or tetanus-reduced diphteria-acellular pertussis (Tdap) vaccine. An appropriately vaccinated woman provides transplacental IgG to the fetus, which decreases the incidence of neonatal tetanus by approximately 95%.