Key points
- Multiple sclerosis (MS) is a chronic degenerative disease of the CNS characterized by demyelination and axonal degeneration in the brain and spinal cord, which are caused by an immune-mediated inflammatory process.
- Impaired vision (due to retrobulbar neuritis) is usually the first manifestation of MS; other neurological deficits appear as the disease progresses. The most common clinical course is characterized by exacerbations followed by periods of complete or incomplete remission.
Epidemiology
- Sex: ♀ > ♂ (3:1)
- Age of onset: 20–40 years of age
- Ethnicity: ↑ prevalence among the white and black population
- Prevalence: 50-300 per 100 000 people (greater among people who live further from the equator)
Etiology
The etiology of multiple sclerosis is unclear; it is believed to develop in genetically predisposed people who have been exposed to certain environmental factors.
- Environmental risk factors
- Low vitamin D levels (insufficient intake, decreased exposure to UV radiation)
Pathophysiology
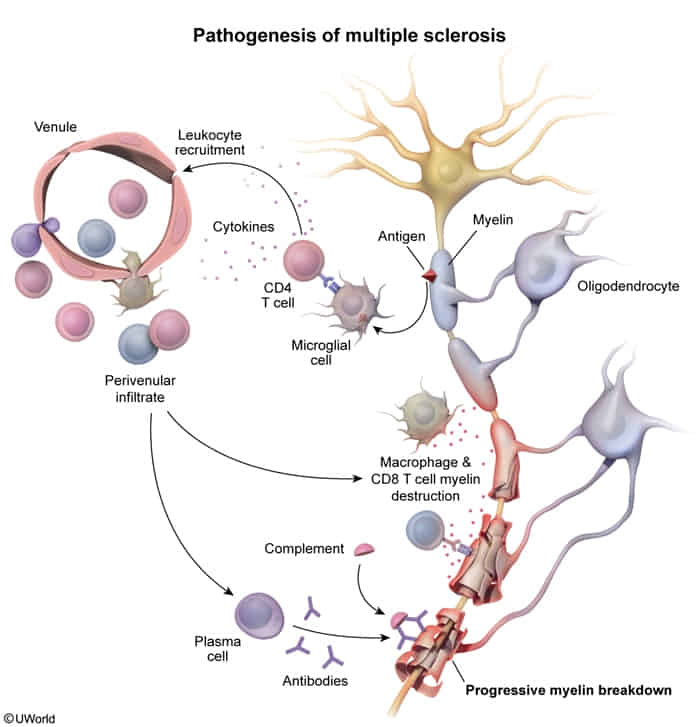
- Autoreactive T cells cross BBB → attack myelin
- Plaques (sclerotic lesions) form in periventricular white matter, optic nerves, brainstem, spinal cord
- Demyelination → ↓ conduction velocity → neurologic deficits
- Acute: inflammation, demyelination
- Chronic: gliosis, axonal loss (irreversible)
Clinical features
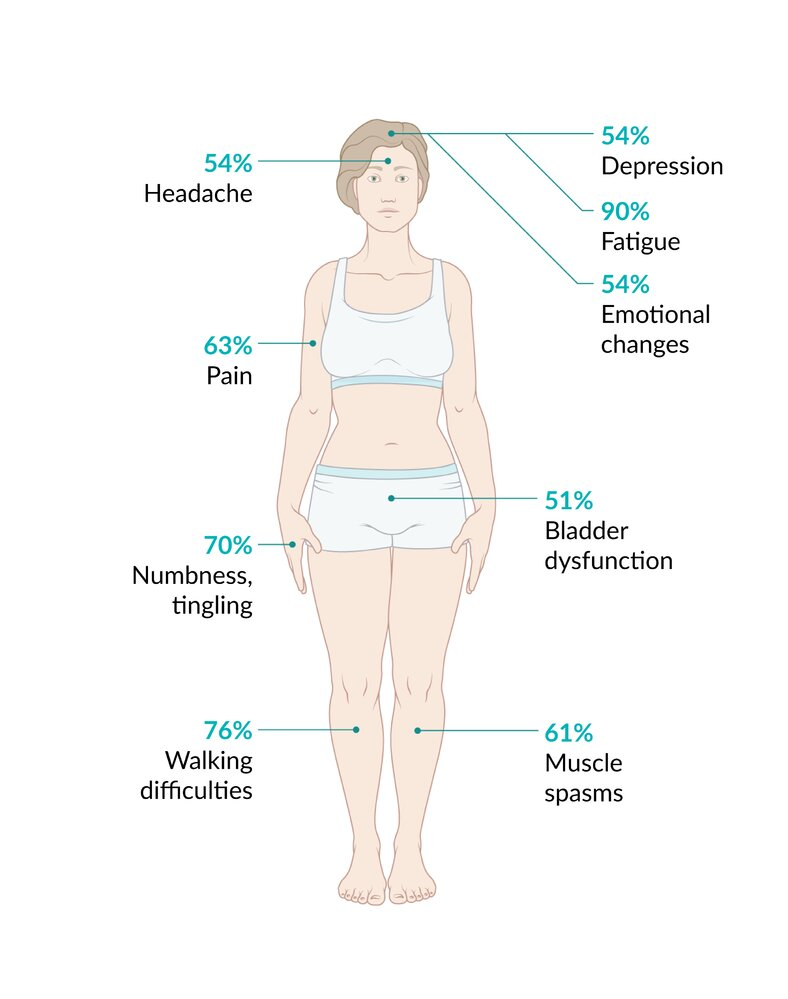
- Optic neuritis
- Most often the earliest manifestation
- Typically unilateral
- Can be painful
- Impaired vision and color blindness
- Relative afferent pupillary defect (Marcus Gunn pupil)
- Internuclear ophthalmoplegia (INO) as a result of a lesion in the medial longitudinal fasciculus (MLF)
- Ipsilateral medial rectus weakness but an intact convergence reflex
- Disconjugate, lateral gaze nystagmus in the contralateral eye
- More frequently bilateral than unilateral
- Demyelination of spinal cord tracts
- Lhermitte sign: a shooting electric sensation that travels down the spine upon flexion of the neck
- Pyramidal tract lesion: upper motor neuron weakness, spasticity, hyperreflexia, positive Babinski sign, impaired gait
- Dorsal spinal column lesion: loss of vibration and fine-touch sensation, numbness, paresthesias, sensory ataxia usually involving the trunk or one or more limbs
- Neuropathic pain
- Absent abdominal reflex
- Cerebellar involvement: poor postural control, imbalance, gait dysfunction, Charcot neurological triad of scanning speech, nystagmus, and intention tremors
- Transverse myelitis
- Asymmetric paraplegia, unilateral sensory loss, bladder dysfunction
- Partial transverse myelitis is a common early manifestation of MS, causing asymmetric neurologic dysfunction below the lesion.
- Cranial nerve palsies: diplopia, facial palsy, trigeminal neuralgia (can be bilateral)
- Trigeminal neuralgia (TN) typically manifests unilaterally.
- Bilateral TN should raise concern for MS, especially in younger patients.
- Autonomic dysfunction: bowel and bladder neurogenic disorders (e.g., urinary incontinence), impaired sexual function
- Changes in mental state: depression, emotional changes, memory deficits, impaired concentration
- Uhthoff phenomenon: a reversible exacerbation of neurological symptoms following an increase in body temperature, e.g., physical exertion, a warm bath, or fever
- Impulse conduction is dependent on temperature. An increase in body temperature presumably worsens impulse conduction in demyelinated nerves.
Tip
MS is a chronic condition that typically manifests in a relapsing-remitting form characterized by episodic CNS dysfunction (exacerbations) with at least partial recovery between episodes.
Diagnostics
- Diagnosis of MS depends on a combination of clinical findings (e.g., optic neuritis, Lhermitte sign, sensory abnormalities, cerebellar signs), imaging, and laboratory results.
- The McDonald Criteria for both DIT and DIS must both be met to confirm a diagnosis of MS:
- Dissemination in time (DIT): the appearance of new CNS lesions over time that can be confirmed clinically, with imaging, or with CSF analysis
- Dissemination in space (DIS): the presence of lesions in different regions of the CNS that can be confirmed clinically or in MRI
Imaging
- MRI: Multiple sclerotic plaques (most commonly found in the periventricular white matter) with finger-like radial extensions (Dawson fingers) related to demyelination and reactive gliosis

 There are extensive demyelinating lesions (plaques) bilaterally, appearing as hyperintensities in the periventricular white matter (green overlay). The finger-like radial extensions of these lesions are called “Dawson fingers.”
There are extensive demyelinating lesions (plaques) bilaterally, appearing as hyperintensities in the periventricular white matter (green overlay). The finger-like radial extensions of these lesions are called “Dawson fingers.”
Additional studies
- CSF examination
- Oligoclonal bands
- Oligoclonal bands manifest due to increased production of multiple nonspecific IgG sub-fractions in the CSF, which are caused by intrathecal inflammation.
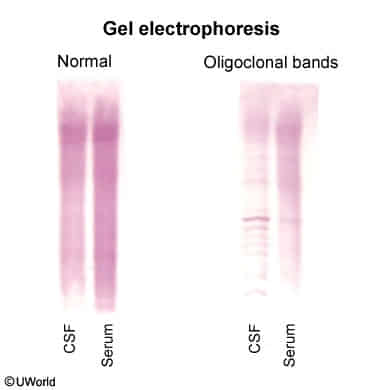
- Oligoclonal bands manifest due to increased production of multiple nonspecific IgG sub-fractions in the CSF, which are caused by intrathecal inflammation.
- Other common findings: moderate lymphocytic pleocytosis, increased myelin basic protein
- Oligoclonal bands
Tip
The presence of multiple oligoclonal bands in CSF and their absence in the blood is highly suggestive of MS.
Treatment
- Acute Flares:
- High-dose IV corticosteroids (e.g., methylprednisolone).
- Plasma exchange for severe, steroid-refractory flares.
- Chronic/Disease-Modifying Therapy (DMT):
- Injectables: Interferon-beta, glatiramer acetate.
- Oral: Dimethyl fumarate, fingolimod.
- Infusions (highly effective): Natalizumab (risk of PML due to JC virus), Ocrelizumab (anti-CD20).
- Symptomatic Management:
- Spasticity: Baclofen, tizanidine.
- Neuropathic pain: Gabapentin, pregabalin, TCAs.
- Fatigue: Amantadine, modafinil.
- Urge incontinence: Anticholinergics (e.g., oxybutynin).