-
Pathophysiology/Etiology
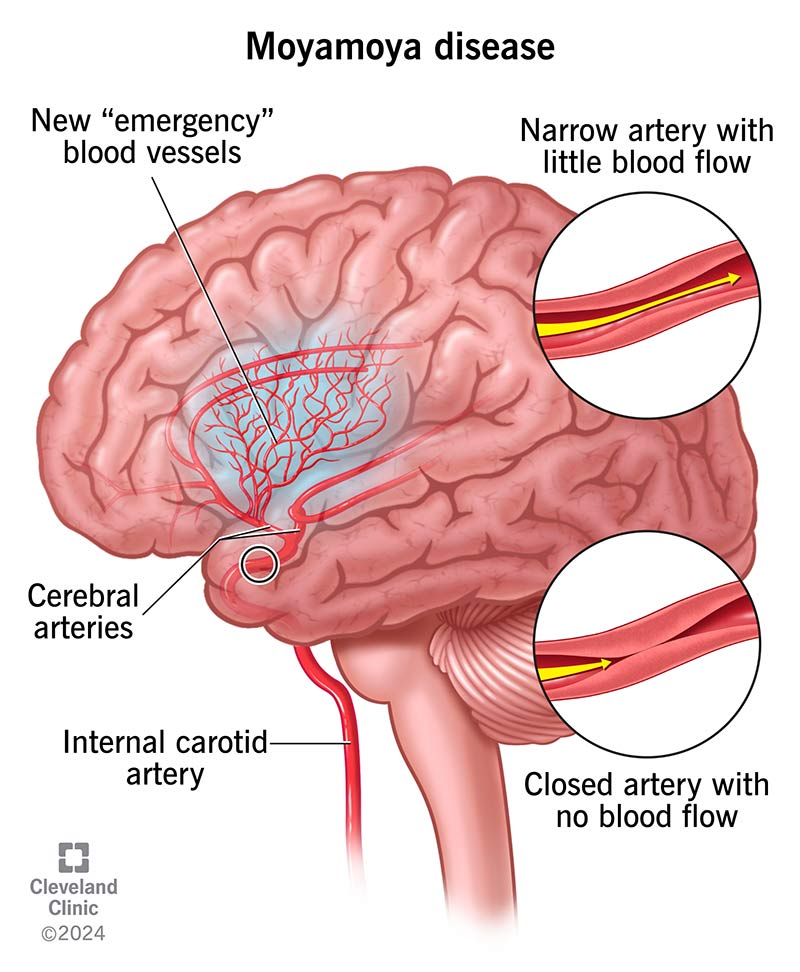
- Chronic, progressive, non-atherosclerotic, non-inflammatory vasculopathy causing bilateral stenosis or occlusion of the terminal internal carotid arteries (ICA) and proximal anterior/middle cerebral arteries (ACA/MCA).
- Leads to the development of a fragile collateral vascular network at the base of the brain, which appears as a “puff of smoke” on angiography (Japanese: moyamoya).
- Cause is unknown (idiopathic), but a genetic link is suspected, with higher prevalence in East Asian populations.
- Moyamoya syndrome refers to similar angiographic findings but is associated with an underlying condition (e.g., sickle cell disease, neurofibromatosis type 1, Down syndrome, cranial irradiation).
-
Clinical Presentation
- Bimodal age distribution: peaks in children (~5-10 years) and adults (~30-50 years).
- Children typically present with ischemic symptoms:
- Transient ischemic attacks (TIAs) or ischemic strokes.
- Symptoms often triggered by hyperventilation (e.g., crying, exercise), leading to hemiparesis, aphasia, or seizures.
- Can also present with headaches, cognitive decline, or involuntary movements.
- Adults have a higher incidence of intracranial hemorrhage from rupture of fragile collateral vessels, often presenting as a hemorrhagic stroke. Ischemic events are also common.
-
Diagnosis
- Cerebral Angiography (Digital Subtraction Angiography - DSA) is the gold standard, showing stenosis/occlusion of terminal ICAs and the classic “puff of smoke” collateral vessels.
- Magnetic Resonance Angiography (MRA) and CT Angiography (CTA) are non-invasive and often used for initial diagnosis and screening, revealing the characteristic arterial stenosis.
- MRI of the brain can show evidence of prior ischemic or hemorrhagic strokes.
-
DDx (Differential Diagnosis)
- Vasculitis of the CNS
- Atherosclerotic cerebrovascular disease (less common in children, different risk factors)
- Reversible cerebral vasoconstriction syndrome (RCVS)
- Fibromuscular dysplasia
- Dissection of carotid or vertebral arteries
-
Management/Treatment
- No curative medical therapy; treatment aims to reduce stroke risk.
- Medical management is adjunctive:
- Antiplatelet agents (e.g., Aspirin) to prevent ischemic events.
- Calcium channel blockers for associated headaches.
- Seizure control with anti-seizure medications if needed.
- Surgical Revascularization is the mainstay of treatment to improve cerebral blood flow and is effective in preventing further strokes.
- Direct bypass (e.g., superficial temporal artery to middle cerebral artery [STA-MCA] bypass): immediately augments blood flow.
- Indirect bypass (e.g., encephaloduroarteriosynangiosis [EDAS]): encourages angiogenesis over time; often used in children.
-
Key Associations/Complications
- Associated Conditions (Moyamoya Syndrome): Neurofibromatosis type 1, sickle cell disease, Down syndrome, prior cranial radiation, hyperthyroidism (Graves’ disease).
- Complications: Recurrent ischemic or hemorrhagic strokes, seizures, cognitive impairment, developmental delay, and potentially fatal brain hemorrhage if untreated. Without treatment, the disease is often progressive.