Pathophysiology & Etiology
- Primary Population: Almost exclusively seen in premature infants, especially those <32 weeks gestation or with very low birth weight (<1500g). The risk of IVH increases as gestational age decreases.
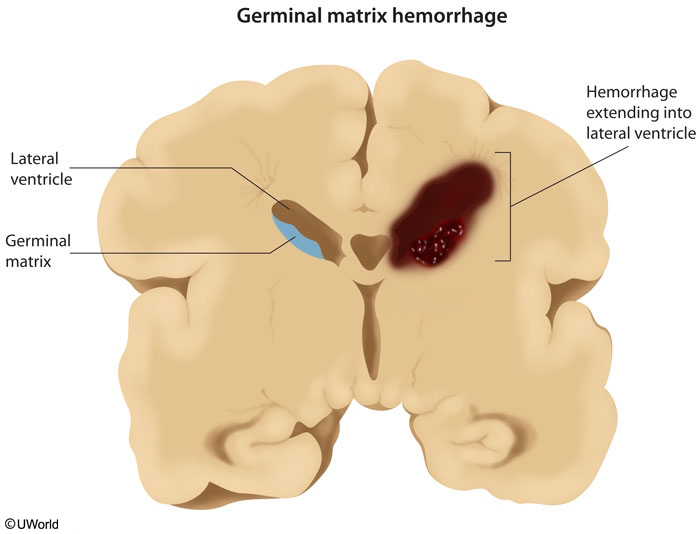
- Source of Bleeding: Rupture of fragile blood vessels in the germinal matrix, a highly vascularized area in the subependymal region that is a source of neurons and glial cells.
- This matrix is prominent between 8 and 28 weeks of gestation and typically involutes by 36 weeks.
- Underlying Cause: The immature cerebral vasculature of preterm infants has impaired autoregulation, making cerebral blood flow pressure-passive. Fluctuations in systemic blood pressure (e.g., due to respiratory distress, hypoxia, hypercarbia, sepsis) can lead to vessel rupture.
- In Term Infants: IVH is rare but can occur, usually originating from the choroid plexus and often associated with trauma or asphyxia.
Clinical Presentation
- Timing: The majority of IVH cases occur within the first 72 hours of life.
- Symptoms: Can range from asymptomatic to catastrophic.
- Asymptomatic: Found on routine screening ultrasound (25-50% of cases).
- Subtle (Saltatory): Gradual neurologic decline with lethargy, hypotonia, decreased spontaneous movement, and subtle changes in vital signs.
- Catastrophic: Acute deterioration with a bulging anterior fontanelle, altered consciousness, seizures, apnea, bradycardia, and a sudden drop in hematocrit.
Diagnosis
- Gold Standard: Cranial ultrasound is the preferred imaging modality. It’s portable, avoids ionizing radiation, and can be performed at the bedside through the anterior fontanelle.
- Screening: Routine screening head ultrasounds are recommended for all infants born at ≤32 weeks gestation, typically performed at 7-14 days of life.
Grading (Papile Classification)
The severity of IVH is graded based on ultrasound findings, which strongly correlates with prognosis.
- Grade I: Hemorrhage confined to the germinal matrix.
- Grade II: IVH without ventricular dilation.
- Grade III: IVH with ventricular dilation (ventriculomegaly).
- Grade IV: IVH with extension into the brain parenchyma (intraparenchymal hemorrhage), often associated with venous infarction.
Management & Complications
- Treatment: There is no specific therapy to stop the hemorrhage. Management is supportive and focuses on:
- Maintaining stable hemodynamics and ventilation.
- Correcting coagulopathy, acidosis, and anemia (e.g., blood transfusion).
- Key Complication: Post-hemorrhagic hydrocephalus (PHH). Blood clots can obstruct CSF flow, leading to progressive ventricular dilation.
- Monitoring: Serial head circumference measurements and follow-up ultrasounds are crucial.
- Treatment of PHH: May require serial lumbar punctures or, if persistent, surgical intervention with a ventriculoperitoneal (VP) shunt.
- Prognosis: Directly related to the grade of the hemorrhage.
- Grades I-II: Often have a good prognosis, similar to infants without IVH.
- Grades III-IV (Severe IVH): Associated with a high risk of mortality and long-term neurologic sequelae, including cerebral palsy, intellectual disability, and seizures. The parenchymal involvement in Grade IV is the main determinant of poor outcomes.