Pathophysiology/Etiology
-
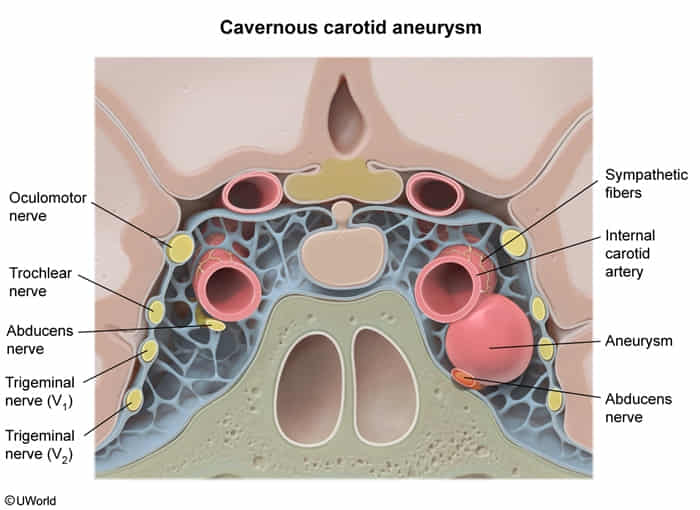
Structures Passing Through cavernous sinus
- Internal Carotid Artery (ICA): Passes directly through the sinus.
- CN VI (Abducens): Runs inside the sinus, lateral to the ICA. Most susceptible to injury due to location.
- Lateral Wall Structures (Superior to Inferior):
- CN III (Oculomotor)
- CN IV (Trochlear)
- CN V1 (Ophthalmic)
- CN V2 (Maxillary)
- Note: CN V3 (Mandibular) and CN II (Optic) do not pass through the cavernous sinus.
-
Definition: Aneurysmal dilation of the internal carotid artery (ICA) segment passing through the cavernous sinus. These are extradural and thus have a low risk of subarachnoid hemorrhage (SAH).
-
Pathophysiology: Symptoms arise from mass effect on adjacent structures within the cavernous sinus, not typically from rupture.
-
Etiology: Often idiopathic. Risk factors include atherosclerosis, hypertension, smoking, female gender, trauma, and infections (mycotic aneurysm).
Clinical Presentation
- Many are asymptomatic and found incidentally.
- Symptomatic Presentation (Cavernous Sinus Syndrome):
- Ophthalmoplegia: Due to compression of cranial nerves (CN).
- CN VI (Abducens) Palsy: Most common finding. Results in lateral rectus weakness and horizontal diplopia.
- CN III (Oculomotor) Palsy: Can cause ptosis and “down and out” eye deviation. May be pupil-sparing initially, as parasympathetic fibers are on the periphery and less susceptible to external compression compared to ischemic injury.
- CN IV (Trochlear) Palsy: Causes vertical diplopia, often noticed when reading or going down stairs.
- Sensory Deficits: Facial pain or numbness in the V1 (ophthalmic) and V2 (maxillary) distributions due to CN V (Trigeminal) compression.
- Horner’s Syndrome: (Ptosis, Miosis, Anhidrosis) from compression of the oculosympathetic fibers that travel with the ICA.
- Headache: Often retro-orbital.
- Ophthalmoplegia: Due to compression of cranial nerves (CN).
Diagnosis
- CTA / MRA: Excellent non-invasive initial tests. Show an enhancing, well-circumscribed lesion within the cavernous sinus, continuous with the ICA. MRA is superior for delineating soft tissue and any thrombus.
- Digital Subtraction Angiography (DSA): Gold standard. Provides definitive diagnosis, shows precise anatomy of the aneurysm neck, and is critical for planning endovascular treatment.
DDx
- Cavernous Sinus Thrombosis: Typically presents more acutely with signs of infection (fever, sepsis), proptosis, and chemosis, often from a facial or sinus infection.
- Meningioma: A solid, dural-based tumor that enhances avidly and uniformly on contrast imaging. May show a “dural tail.”
- Tolosa-Hunt Syndrome: Idiopathic granulomatous inflammation of the cavernous sinus causing painful ophthalmoplegia. Diagnosis of exclusion, shows dramatic improvement with steroids.
- Carotid-Cavernous Fistula (CCF): Abnormal connection between the ICA and cavernous sinus. Presents with the classic triad of pulsatile exophthalmos, ocular bruit, and chemosis. Often post-traumatic.
Management/Treatment
- Asymptomatic/Small Aneurysms: Conservative management with serial imaging (e.g., MRA) to monitor for growth.
- Symptomatic/Large/Growing Aneurysms:
- Endovascular Therapy (First-Line):
- Flow-Diverting Stent: A stent placed across the aneurysm neck to promote thrombosis within the aneurysm while maintaining flow in the parent vessel.
- Coil Embolization: Packing the aneurysm sac with platinum coils to induce thrombosis. May be combined with stenting.
- Parent Artery Occlusion: Therapeutic occlusion of the ICA, considered if collateral circulation is adequate (assessed by balloon test occlusion).
- Microsurgical Clipping: Rarely performed due to the high morbidity associated with operating within the cavernous sinus.
- Endovascular Therapy (First-Line):
Key Associations/Complications
- Cavernous Sinus Syndrome: The primary clinical manifestation.
- Carotid-Cavernous Fistula (CCF): Can occur if the aneurysm ruptures into the surrounding venous sinus.
- Thromboembolism: Clot from within the aneurysm can embolize distally, causing a TIA or stroke.
- Epistaxis: Rare but life-threatening complication if the aneurysm erodes through the sphenoid bone into the sphenoid sinus.