Tip
- The superior gluteal nerve originates from the L4, L5, and S1 roots.
- Gluteus medius, gluteus minimus, tensor fascia latae
- thigh/hip abduction
- The inferior gluteal nerve arises from L5, S1, and S2.
- Gluteus maximus
- Thigh/hip extension
- The posterior cutaneous nerve comes from S1, S2, and S3.
- The pudendal nerve is derived from S2, S3, and S4.
- The sciatic nerve, being the largest, includes roots from L4 to S3.
- Obturator nerve
- thigh adduction
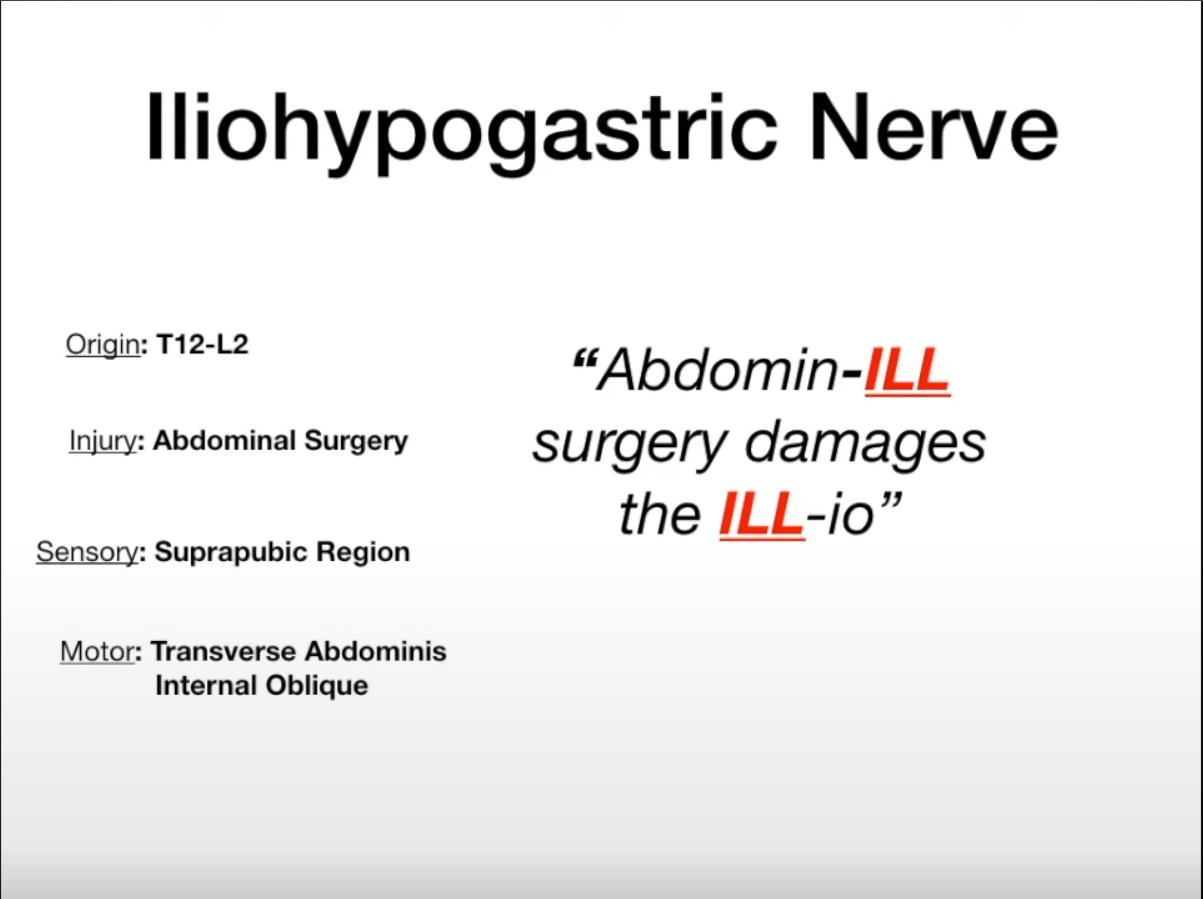
Iliohypogastric Nerve (T12-L1)
- Motor: Internal oblique and transversus abdominis muscles (abdominal wall support and compression).
- Sensory: Skin over suprapubic region and lateral gluteal/iliac crest region.
- Clinical: Injury (e.g., during abdominal surgery like appendectomy or hernia repair) → weakness of anterior abdominal wall (predisposing to direct inguinal hernia), altered sensation in suprapubic/inguinal region.
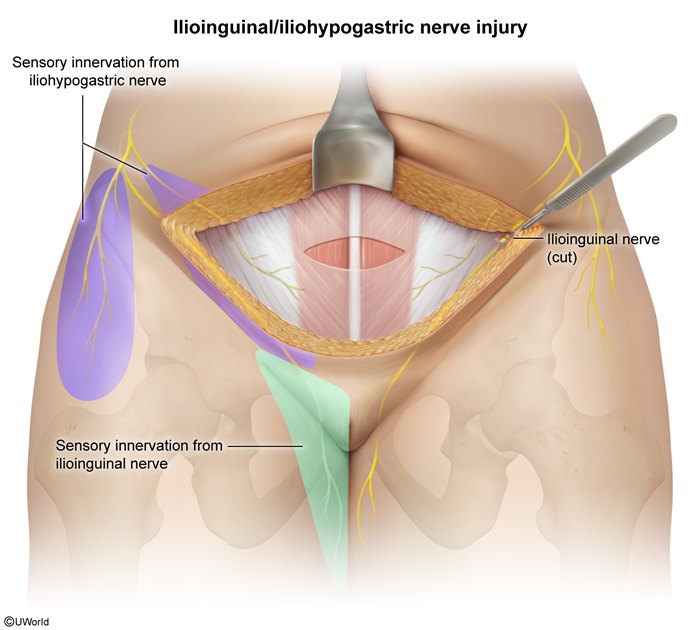
Ilioinguinal Nerve (L1)
- Motor: Internal oblique and transversus abdominis muscles.
- Sensory: Skin of upper medial thigh, root of penis and anterior scrotum (males) or mons pubis and labia majora (females). Travels through inguinal canal.
- Clinical: Injury (e.g., during inguinal hernia repair) → sensory loss in the distribution, pain. Can be entrapped.
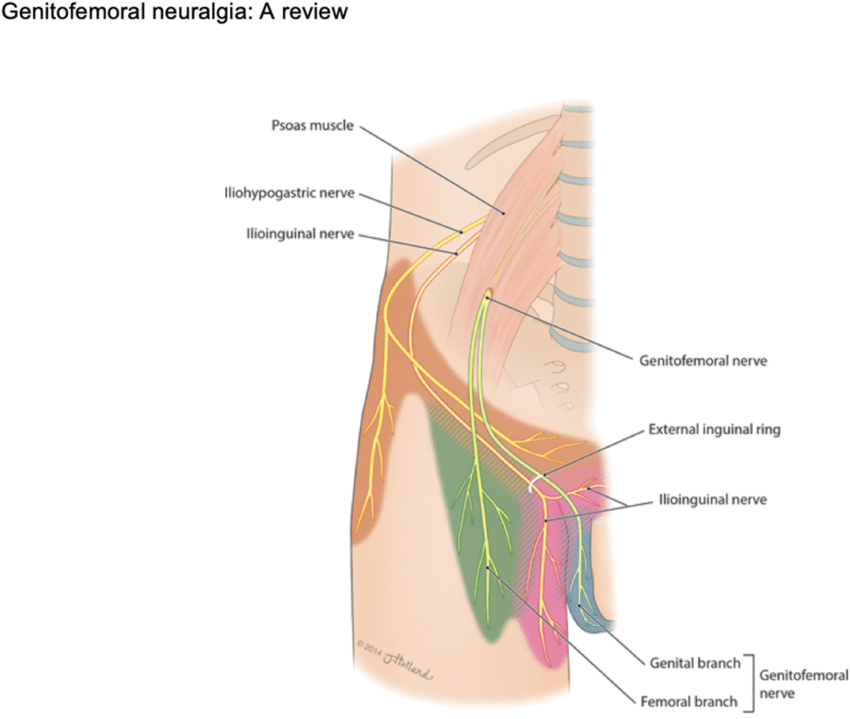
Genitofemoral Nerve (L1-L2)
- Motor:
- Genital branch: Cremaster muscle (males – testicular elevation, cremasteric reflex).
- Femoral branch: None (sensory only).
- Sensory:
- Genital branch: Skin of anterior scrotum (males) or mons pubis and labia majora (females).
- Femoral branch: Skin over femoral triangle/upper anterior thigh.
- Clinical: Injury (e.g., during inguinal or femoral surgery, appendectomy) → loss of cremasteric reflex, sensory loss in distribution.
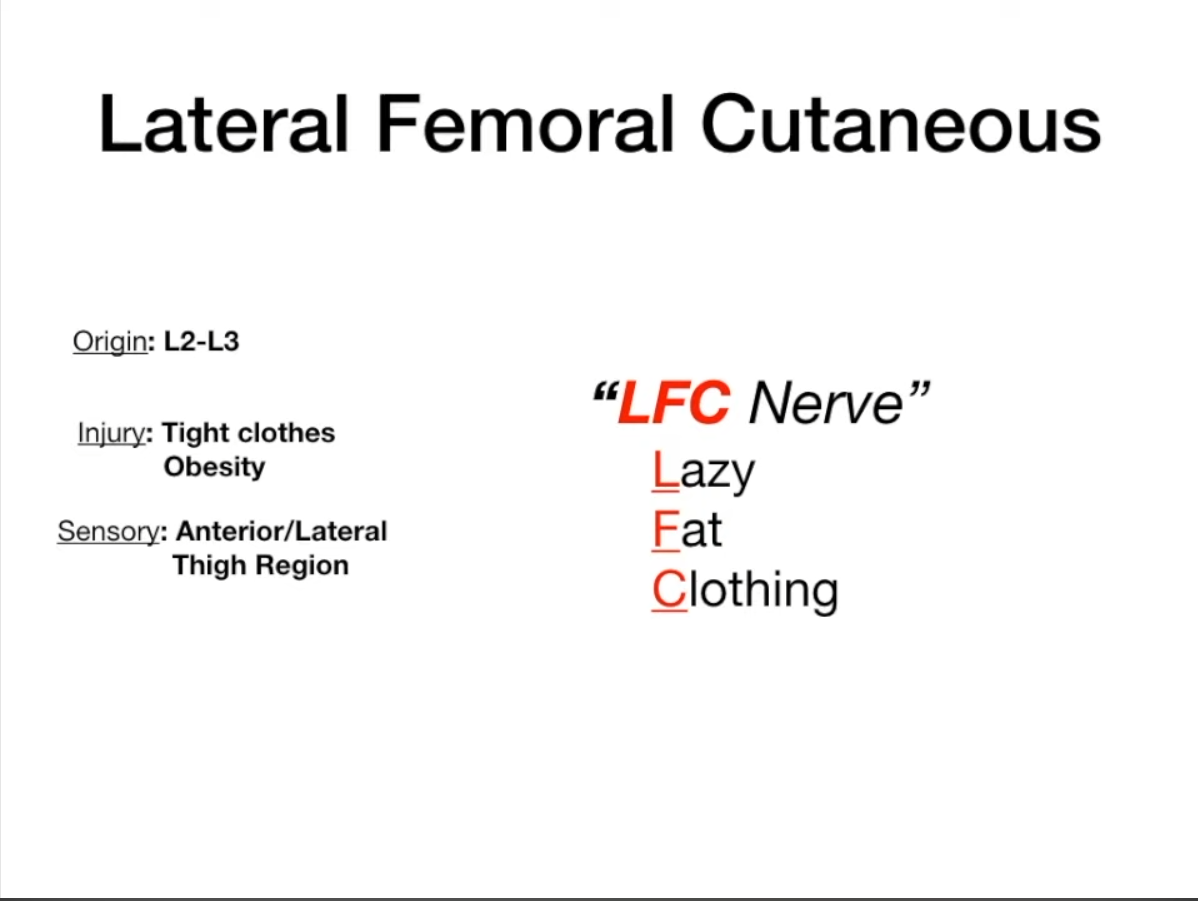
Lateral Femoral Cutaneous Nerve (L2-L3)
- Motor: None.
- Sensory: Skin on anterolateral aspect of the thigh.
- Clinical: Entrapment under inguinal ligament (common) → Meralgia Paresthetica (pain, burning, numbness over lateral thigh). Risk factors: obesity, pregnancy, tight clothing.
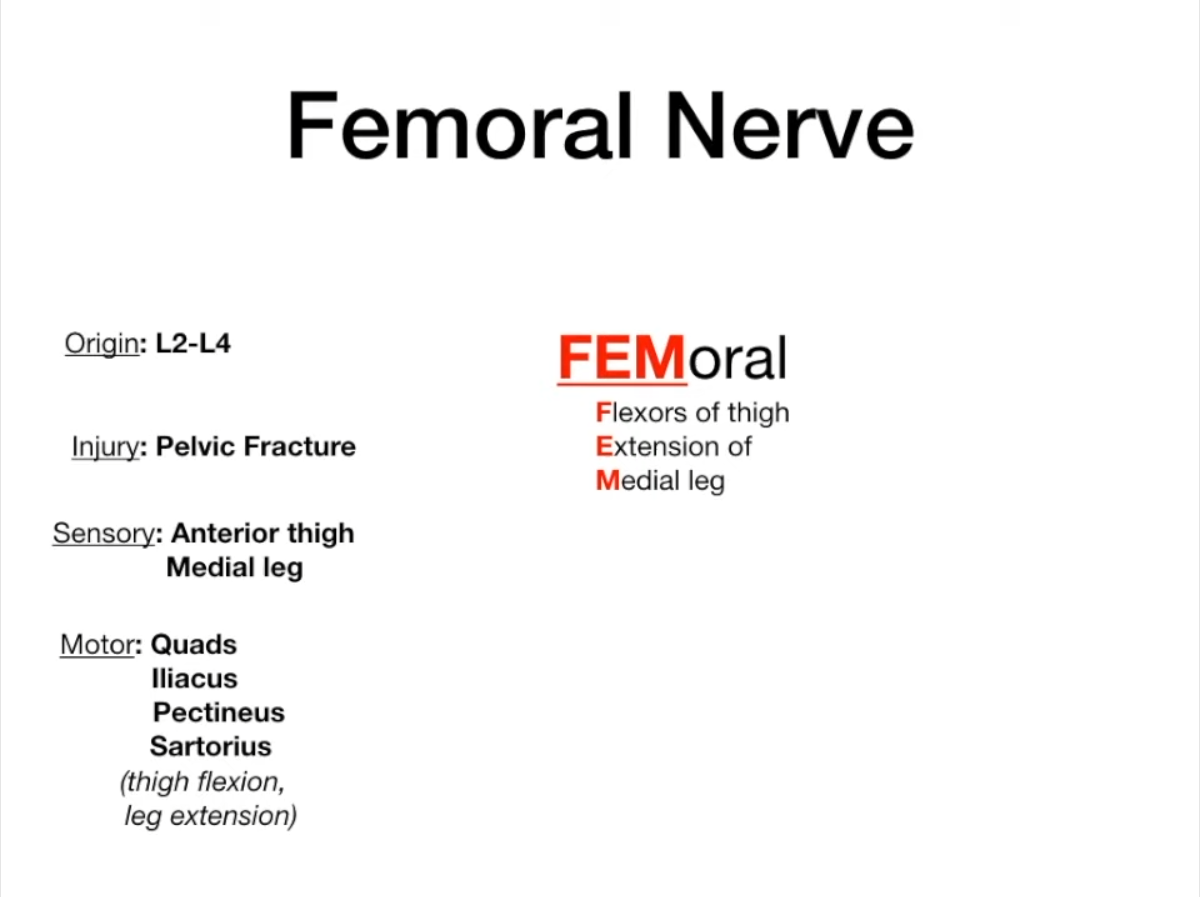
Femoral nerve (L2-L4)
- Etiology
- Retroperitoneal hematoma: High yield in pts on anticoagulants (Warfarin/Heparin) w/ groin pain.
- Lithotomy position: Prolonged pelvic surgery.
- Diabetes: Diabetic amyotrophy.
- Trauma: Pelvic fracture, catheterization.
- Motor: Anterior thigh compartment muscles (quadriceps femoris for knee extension; sartorius, pectineus, iliacus for hip flexion).
- Sensory: Anterior thigh, medial leg and foot (via saphenous nerve).
- Clinical: Injury → impaired knee extension, loss of patellar reflex, sensory loss to anterior thigh & medial leg/foot.
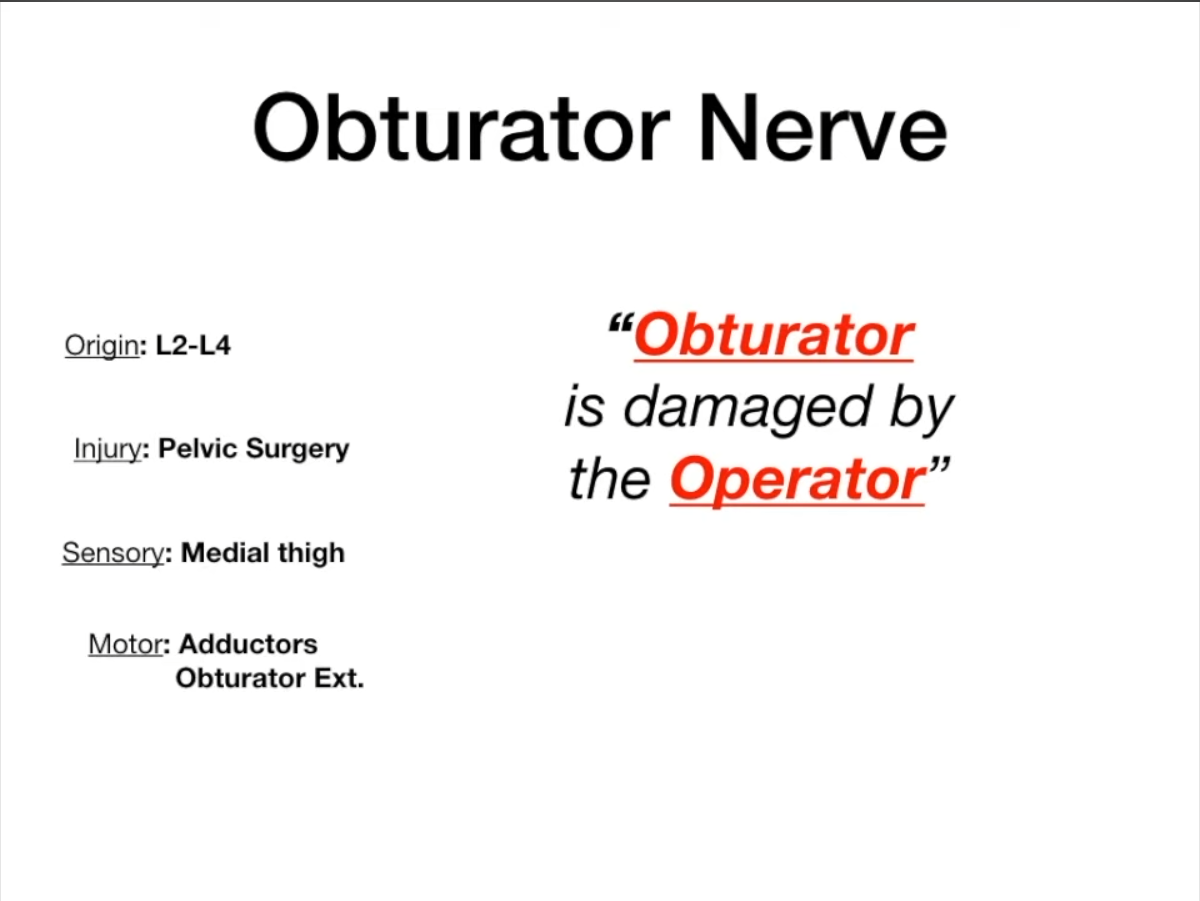
Obturator nerve (L2-L4)
- Motor: Medial thigh compartment (adductor muscles: adductor longus, brevis, magnus adductor part; gracilis, obturator externus).
- Sensory: Medial thigh.
- Clinical: Injury → weakened thigh adduction, sensory loss to medial thigh.
Sciatic Nerve (L4-S3)
- General: Largest nerve; bifurcates into Tibial and Common Peroneal nerves (typically in lower thigh/popliteal fossa).
- Motor (direct branches): Posterior thigh compartment (hamstrings: semitendinosus, semimembranosus, biceps femoris long head) for knee flexion & hip extension. Ischial part of adductor magnus.
- Sensory: No direct sensory to skin; supplied via its branches.
- Clinical: Injury (e.g., piriformis syndrome, hip dislocation) → weakness in hamstrings and all muscles below knee; foot drop (if common peroneal component affected significantly).
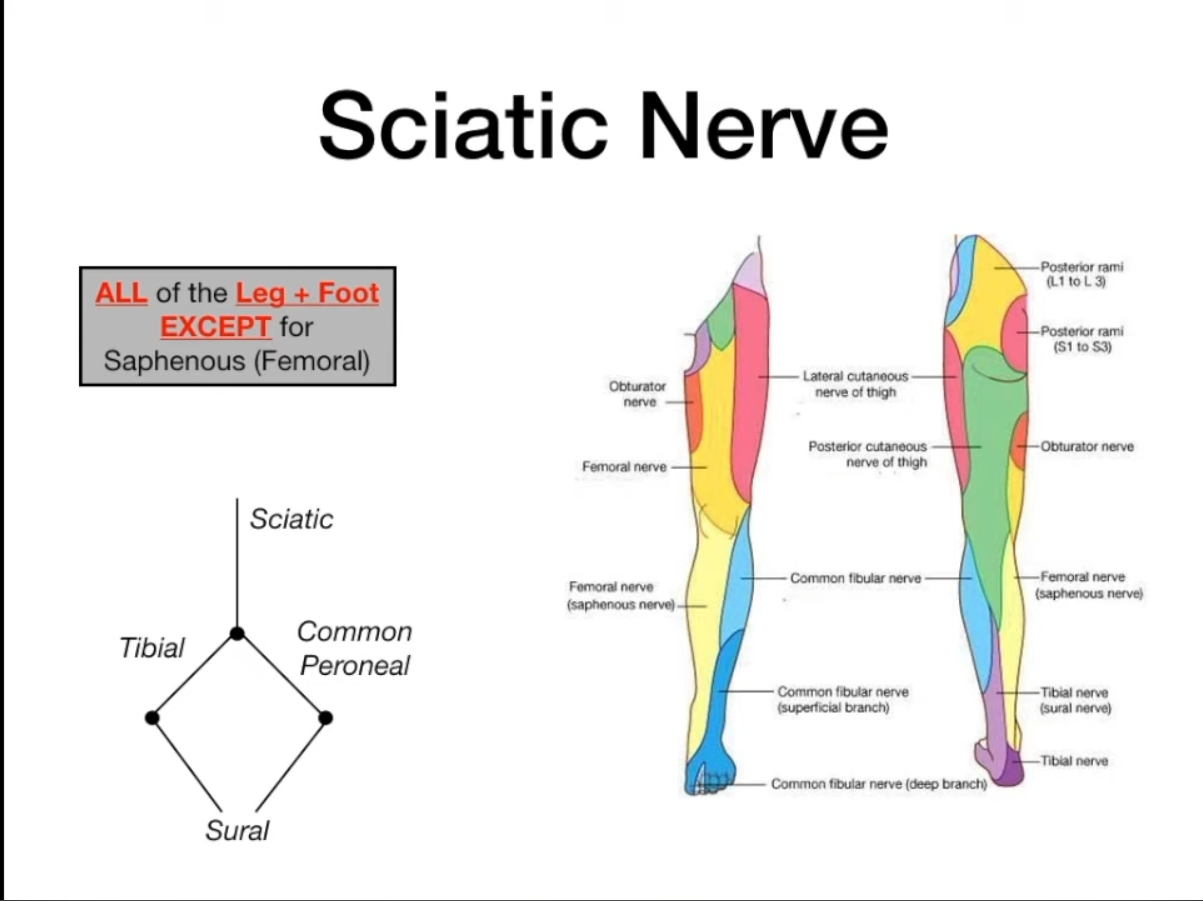
Tibial Nerve (L4-S3) (branch of Sciatic)
- Motor: Posterior compartment of leg (gastrocnemius, soleus, plantaris for plantarflexion; popliteus; tibialis posterior for inversion & plantarflexion; FHL, FDL for toe flexion). Most intrinsic foot muscles (via medial & lateral plantar nerves).
- Sensory: Posterolateral leg (via sural nerve, often with common peroneal contribution), sole of foot (via medial & lateral plantar nerves), heel (via medial calcaneal branches).
- Clinical: Injury → inability to plantarflex or invert foot, loss of toe flexion, sensory loss to sole. “Tip-toe” if proximal. Tarsal tunnel syndrome (entrapment at ankle).
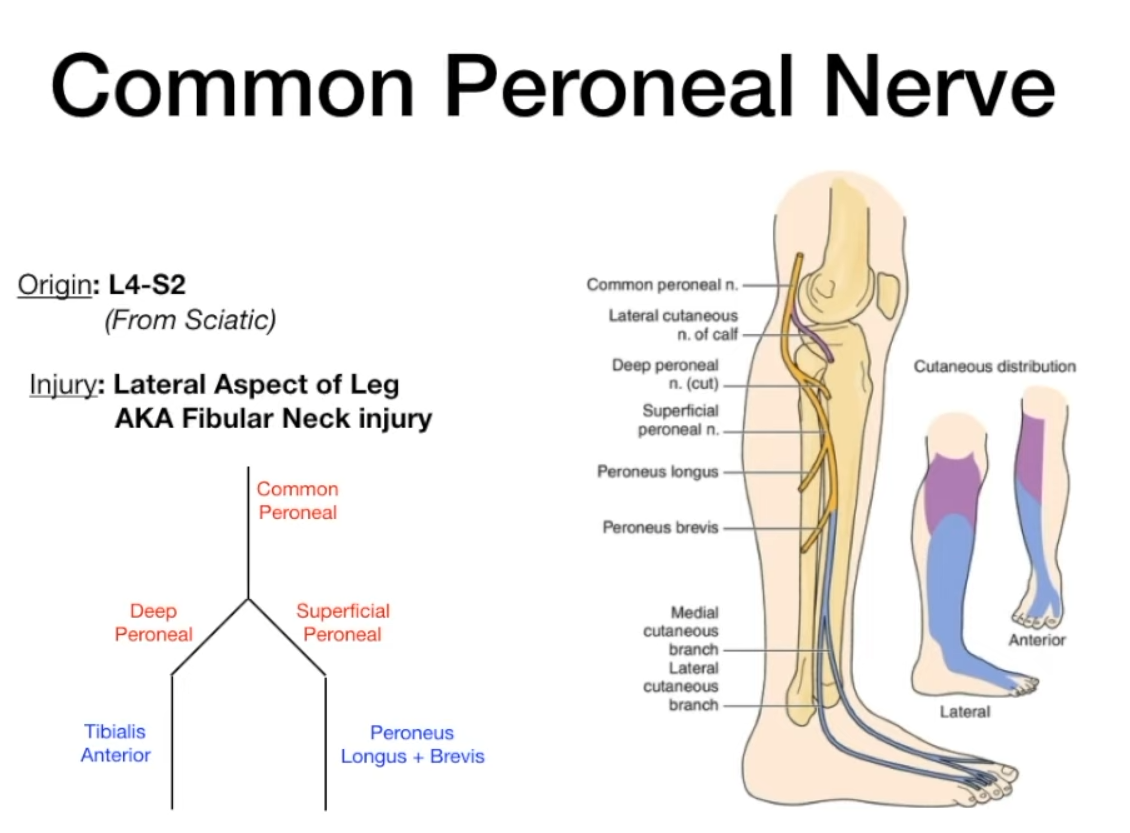
Common Peroneal (Fibular) Nerve (L4-S2) (branch of Sciatic)
- Motor (direct branch): Short head of biceps femoris.
- Sensory: Lateral sural cutaneous nerve (skin on upper anterolateral leg).
- Divides into: Superficial and Deep Peroneal nerves.
- Clinical: Most frequently injured nerve in lower limb, esp. at fibular neck. Injury → Foot drop (loss of dorsiflexion and eversion), sensory loss over lateral leg & dorsum of foot.
- Superficial Peroneal Nerve:
- Motor: Lateral compartment of leg (peroneus longus & brevis for eversion).
- Sensory: Anterolateral distal leg & dorsum of foot (except 1st web space).
- Deep Peroneal Nerve:
- Motor: Anterior compartment of leg (tibialis anterior for dorsiflexion & inversion; EHL, EDL for toe extension). Extensor digitorum brevis & extensor hallucis brevis in foot.
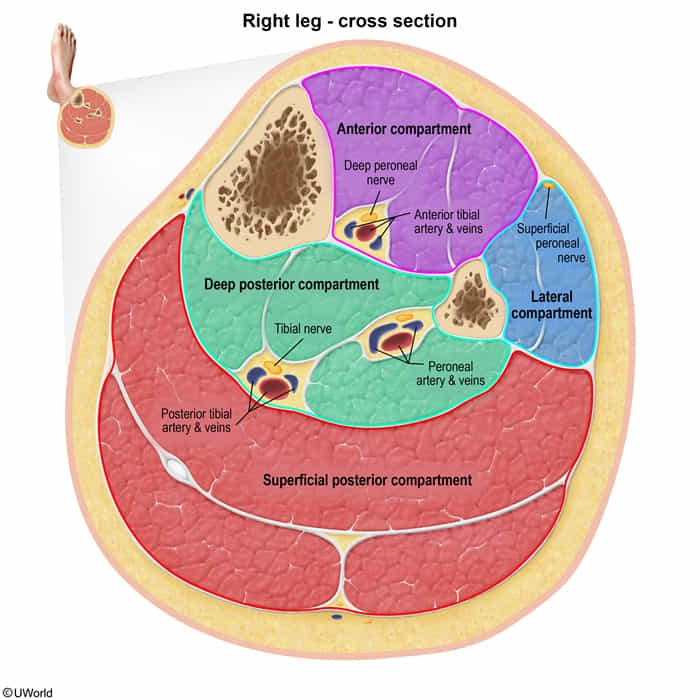
- Sensory: First dorsal web space (b/w 1st & 2nd toes).
- Motor: Anterior compartment of leg (tibialis anterior for dorsiflexion & inversion; EHL, EDL for toe extension). Extensor digitorum brevis & extensor hallucis brevis in foot.
Mnemonic
“Drop and Deep” (both start with “D”)
| Feature | Common Peroneal | Deep Peroneal | Superficial Peroneal |
|---|---|---|---|
| Foot Drop | YES | YES | NO |
| Foot Eversion | Impaired | Spared | Impaired |
| Foot Inversion | Spared | Spared | Spared |
| Plantarflexion | Spared | Spared | Spared |
| Sensory Loss | Anterolateral leg + Dorsum of foot | Webspace between 1st/2nd toes | Dorsum of foot (spares webspace) |
| Classic Cause | Fibular neck fracture/compression | Anterior compartment syndrome | Trauma to lateral compartment |
Superior Gluteal Nerve (L4-S1)
- Motor: Gluteus medius, gluteus minimus, tensor fascia lata (hip abduction, medial rotation; pelvic stabilization).
- Sensory: Generally considered motor, though some sources note hip joint capsule sensation.
- Clinical: Injury → Trendelenburg gait/sign (pelvis sags on contralateral side when standing on affected leg), waddling gait.
- Causes
- Iatrogenic injury from intramuscular injection in the upper medial gluteal region
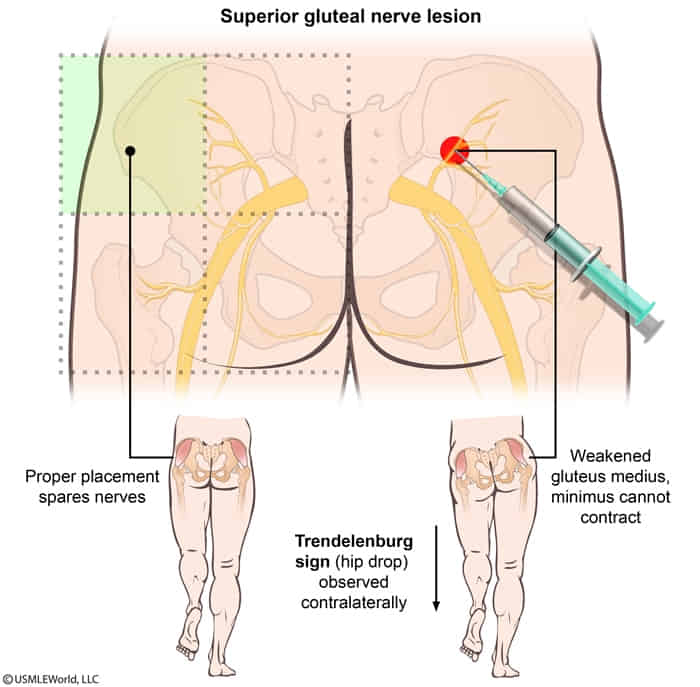
- Correct buttock injection site
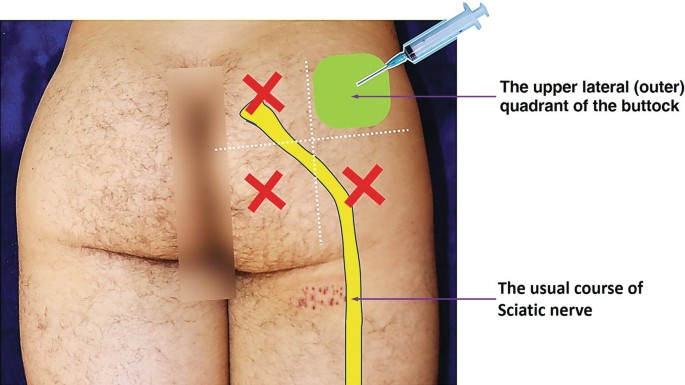
- Correct buttock injection site
- Iatrogenic injury from intramuscular injection in the upper medial gluteal region
- Motor deficits
- Paralysis of gluteus medius and minimus, tensor fascia lata → impaired hip abduction
- Positive Trendelenburg sign: lateral pelvic drop towards the opposite (healthy) side
- Causes
Inferior Gluteal Nerve (L5-S2)
- Motor: Gluteus maximus (powerful hip extension, e.g., rising from sit, climbing stairs).
- Sensory: None primarily.
- Clinical: Injury → difficulty rising from seated position, climbing stairs, “gluteus maximus lurch” (backward trunk lean during stance phase).
Posterior Cutaneous Nerve of Thigh (S1-S3)
- Motor: None.
- Sensory: Skin of posterior thigh and popliteal fossa, inferior gluteal region, parts of perineum.
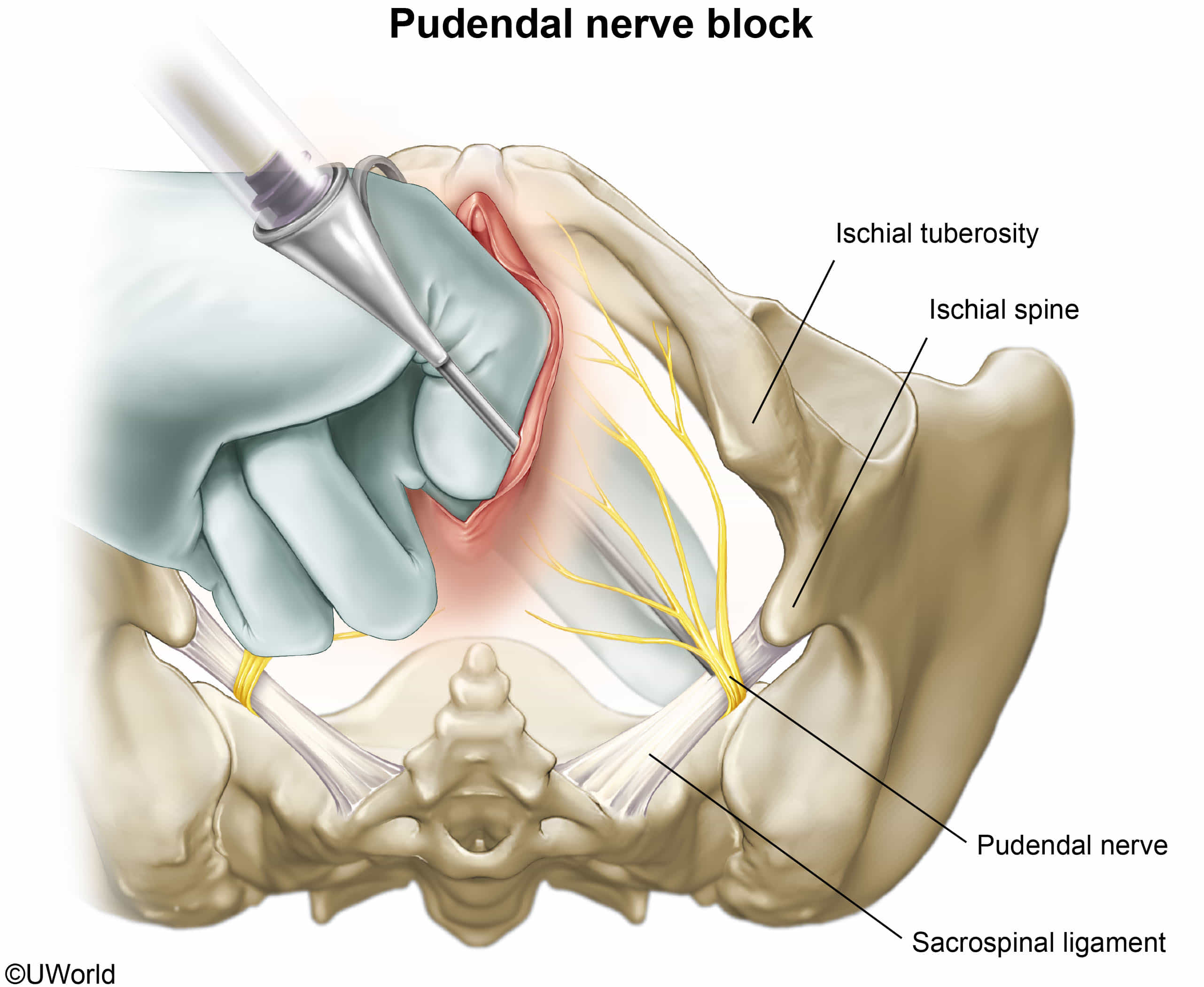
Pudendal nerve
- Motor: Muscles of perineum, external urethral sphincter, external anal sphincter.
- Sensory: Skin of perineum, penis/clitoris, posterior scrotum/labia.
- Clinical: Injury (e.g., childbirth, cycling, pelvic surgery) → fecal/urinary incontinence, sexual dysfunction, perineal pain. Pudendal nerve block used for obstetric analgesia.
- Pudendal nerve block: injection of a local anesthetic into the pudendal canal to block transmission within the pudendal nerve
- Most commonly used during childbirth prior to an episiotomy or during surgical procedures involving the perineum
- The ischial spine is used as a landmark for injection.