Common joint dislocations
Shoulder (Glenohumeral) Dislocation
-
Patho/Etiology
- Most commonly dislocated major joint due to the shallow glenoid fossa.
- Anterior (>95%): Most common type. Caused by a blow to an abducted, externally rotated, and extended arm (e.g., throwing a football, blocking a shot).
- Posterior (2-4%): Often missed. Classic causes are seizures, electrocution, or a direct blow to the anterior shoulder.
-
Clinical Presentation
- Anterior: Arm is held in slight abduction and external rotation. The acromion appears prominent, with a "squared-off" or flattened deltoid contour.
- Posterior: Arm is held in adduction and internal rotation. The anterior shoulder appears flattened with a prominent coracoid process.
-
Diagnosis
- X-ray (AP and axillary/scapular "Y" views): Confirms the direction of dislocation.
- Anterior Dislocation Associated Lesions:
- Hill-Sachs lesion: Compression fracture of the posterolateral humeral head.
- Bankart lesion: Avulsion of the anteroinferior glenoid labrum.
-
Management
- Immediate closed reduction after neurovascular exam and pre-reduction X-rays (Hippocratic technique).

- Immobilization (sling) followed by physical therapy.
- Surgery may be needed for recurrent dislocations, especially in young athletes.
- Immediate closed reduction after neurovascular exam and pre-reduction X-rays (Hippocratic technique).
-
Key Complications
- Axillary nerve injury (most common): Presents with deltoid weakness (impaired abduction) and loss of sensation over the lateral shoulder ("regimental badge" area). Often transient and resolves with reduction.
- Rotator cuff tear: More common in older patients.
- Recurrent dislocation: Common, especially in younger, active individuals.
Mnemonic
拍拍肩膀说:嗨H
拍拍屁股说:啊A
Hip Dislocation
-
Patho/Etiology
- Requires significant force; often from motor vehicle accidents (dashboard injury) or falls from a height.
- Posterior (>90%): Femoral head is forced posteriorly out of the acetabulum.
- Anterior (<10%): Usually from forced abduction.
-
Clinical Presentation
- Posterior: The affected limb is shortened, adducted, and internally rotated. This is the classic, high-yield presentation.
- Anterior: Limb is abducted and externally rotated.
-
Diagnosis
- X-ray (AP pelvis): Confirms diagnosis. In posterior dislocation, the femoral head appears smaller than the contralateral side. A CT scan is often done post-reduction to check for associated fractures.
-
Management
- Orthopedic emergency.
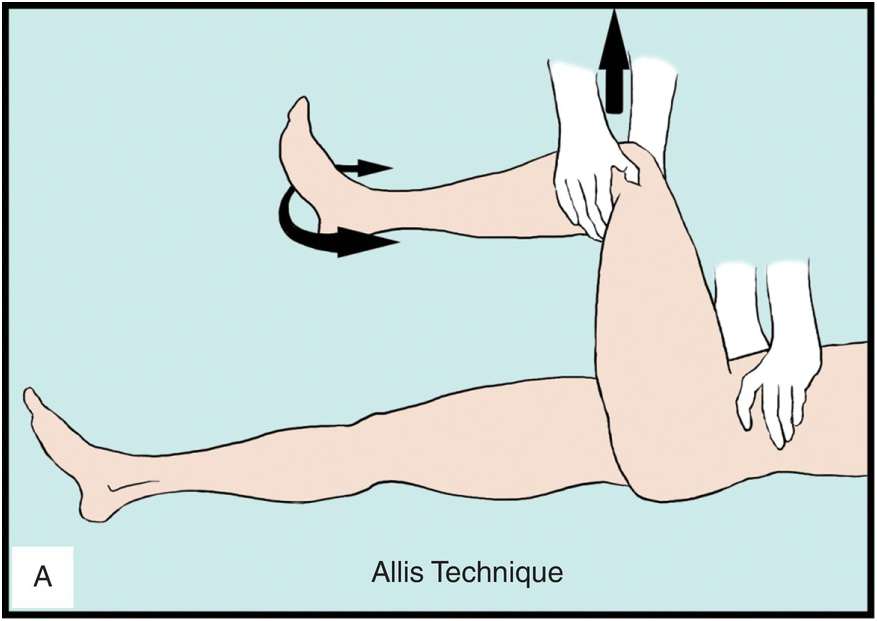
- Prompt closed reduction under sedation to decrease the risk of avascular necrosis (Allis technique).
- Open reduction if closed reduction fails or if there are associated fractures.
-
Key Complications
- Avascular necrosis (AVN) of the femoral head: The most serious complication; risk increases with time to reduction.
- Sciatic nerve injury: Common with posterior dislocations, presenting with foot drop (impaired dorsiflexion).
- Post-traumatic arthritis: The most common long-term complication.
Elbow Dislocation
-
Patho/Etiology
- Second most common major joint dislocation in adults; most common in children.
- Usually caused by a fall on an outstretched hand (FOOSH) with the elbow in extension.
- Posterior dislocation is the most common type.
-
Clinical Presentation
- Presents with severe pain, swelling, and inability to bend the elbow. The olecranon is prominent posteriorly.
-
Diagnosis
- X-ray (AP and lateral): Confirms dislocation. Important to assess for associated fractures.
- "Terrible triad" of the elbow: A complex dislocation involving a posterior dislocation, a radial head fracture, and a coronoid process fracture.
-
Management
- Immediate closed reduction after a careful neurovascular exam.
- Post-reduction, the elbow is splinted in flexion (around 90 degrees). Early range of motion is crucial to prevent stiffness.
-
Key Complications
- Neurovascular injury:
- Brachial artery injury: Can be limb-threatening. Always check for distal pulses before and after reduction.
- Median and ulnar nerve injuries are also common.
- Compartment syndrome: A risk, especially with associated fractures.
- Contracture/Stiffness: Loss of terminal extension is a very common long-term complication.
- Neurovascular injury:
Knee (Tibiofemoral) Dislocation
-
Patho/Etiology
- A rare but limb-threatening orthopedic emergency, often from high-energy trauma (MVA, falls).
- Can occur with lower energy in morbidly obese individuals.
- Up to 50% of knee dislocations spontaneously reduce before evaluation, so a high index of suspicion is required.
-
Clinical Presentation
- Gross deformity and instability of the knee. If reduced, may present with significant swelling and multi-ligamentous instability.
-
Diagnosis
- Based on clinical suspicion, even if the joint is reduced.
- Ankle-brachial index (ABI): A crucial screening tool. An ABI <0.9 warrants further vascular imaging.
- CT angiography: To rule out vascular injury.
-
Management
- Immediate reduction. Do not delay for imaging if there are signs of vascular compromise.
- Careful and repeated neurovascular checks are critical.
- Admission for observation and serial exams is standard.
-
Key Complications
- Popliteal artery injury (up to 40%): High risk of amputation if not recognized and treated promptly (within 8 hours). This is the most feared complication.
- Common peroneal (fibular) nerve injury: Presents with foot drop and numbness on the dorsum of the foot.
- Multiple ligament tears (ACL, PCL, etc.): Nearly always present and require surgical reconstruction.