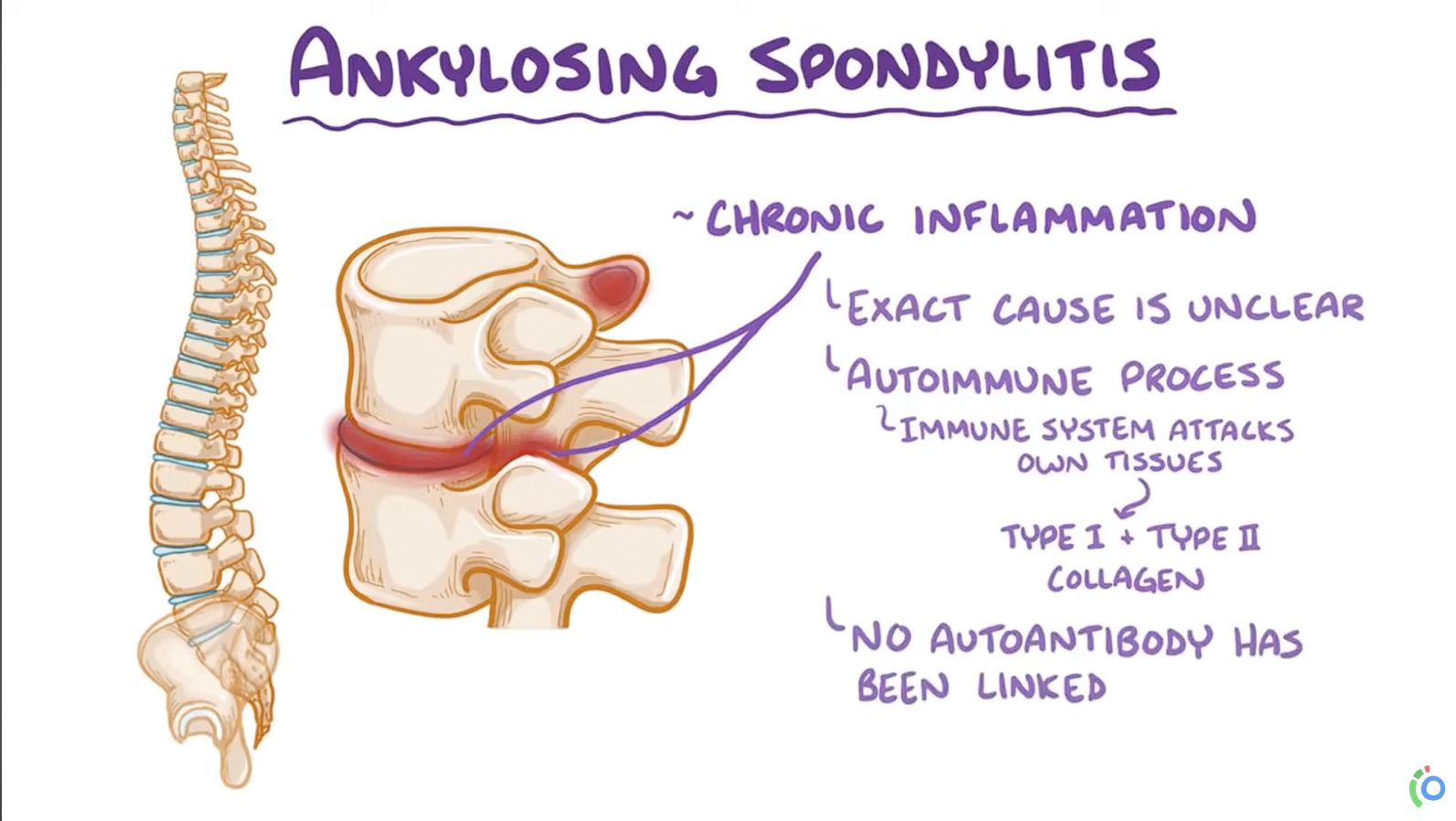
Ankylosing spondylitis
Epidemiology
Etiology
- Genetic predisposition: 90–95% of patients are HLA-B27 positive.
Pathophysiology
- AS is distinct from rheumatoid arthritis:
- AS → simultaneous bone erosion AND new bone formation.
- Rheumatoid arthritis → primarily only erosions.
- Initial Pathogenesis (Inflammatory Phase):
- Driven partly by inflammatory cytokines (e.g., tumor necrosis factor (TNF), IL-17) → activation of osteoclast precursor cells → bony erosions.
- Bony erosions occur primarily in vertebral bodies → destruction of the trabecular microarchitecture → increased risk for secondary osteoporosis and compression fractures.
- Reparative Process (Post-Inflammation):
- Inflammation subsides → reparative process begins → excessive new bone formation.
- New bone formation occurs especially where fat metaplasia fills previously eroded sites.
- In contrast to erosion, bone formation occurs primarily at the periosteum-cartilage junction → manifests as bridging syndesmophytes in the vertebral column.
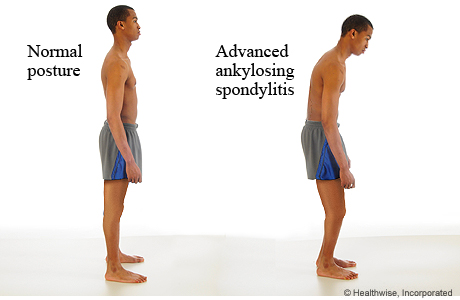
- Bridging syndesmophytes → spinal rigidity → postural alterations → increased risk of fracture.
- Initiation of innate immune response
- Release of cytokines (TGF-beta and TNF-α) and interleukins (IL-17 and IL-23)
- Infiltration of paravertebral and sacroiliac entheses with macrophages, CD4 T cells, and CD8 T cells
- Enthesitis: an inflammation of the enthesis (the point at which a tendon attaches to bone). Typically seen in patients with ankylosing spondylitis, psoriatic arthritis, enthesitis-associated juvenile idiopathic arthritis, or reactive arthritis. Commonly affected sites include the spine, Achilles tendon, plantar fascia, and supraspinatus tendon.

- Chronic enthesitis leads to:
- Erosion of the iliac part of the sacroiliac joints
- Vertical formation of syndesmophytes along the spinal ligament or around the annulus fibrosus of the intervertebral discs
- Fusion of syndesmophytes → ankylosis of intervertebral discs and vertebral bodies
Clinical features
- Inflammatory back pain (sacroiliitis)
- Insidious onset at age <40
- Morning stiffness > 30 minutes that improves with activity
- Pain is independent of positioning
- Relieved with exercise, worse with rest (overnight & in the morning)
- Relieved with activity & warm showers
- Nocturnal pain
- Reduced chest expansion & spinal mobility
- Stiff or stooped posture
- Tenderness at spine, sacroiliac joints & peripheral tendon insertions (eg, Achilles)
- Enthesitis (tenderness at tendon insertion sites)
- Dactylitis (swelling of fingers & toes)
- Uveitis
Diagnostics
AS is a seronegative spondyloarthropathy, and there are no serologic tests to confirm the diagnosis.
Laboratory findings
- Elevated ESR & CRP
- HLA-B27: Positive in 90–95% of patients with axial spondyloarthritis
- Autoantibodies (e.g., rheumatoid factor, antinuclear antibodies) are negative
X-ray
- Sacroiliitis: bone erosions, subchondral sclerosis, eventual bony fusion (ankylosis)
- Bridging syndesmophytes: ossification at vertebral body margins (bamboo spine)