Epidemiology
Etiology
- Family: Orthomyxovirus (Enveloped, negative-sense ssRNA, segmented genome).
- Segmented genome allows for genetic reassortment.
- Key Surface Antigens:
- Hemagglutinin (HA): Binds sialic acid receptors on host cells → viral entry.
- Neuraminidase (NA): Cleaves sialic acid to release progeny virus → viral exit.
- Genetic Variation:
- Antigenic Drift: Minor changes due to random point mutations in HA or NA. Causes seasonal epidemics. Reason for annual vaccine updates.
- Antigenic Shift: Major change due to reassortment of RNA segments between two viruses (e.g., human + swine flu) infecting the same cell. Causes Pandemics (Shift = Segments). t
Pathophysiology
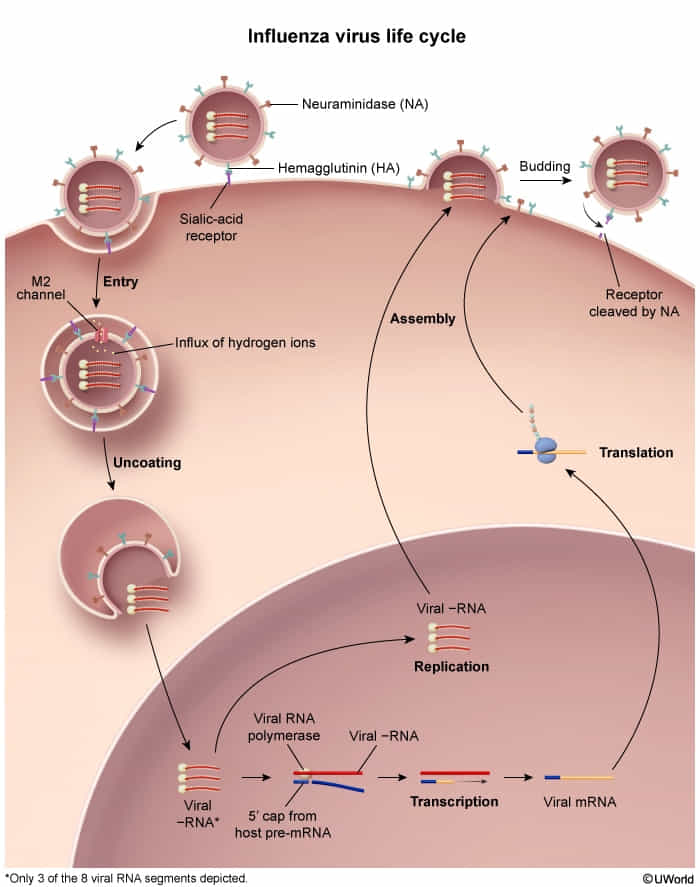
- Replication cycle
- Influenza viruses bind to the respiratory tract epithelium.
- Viral hemagglutinin (H) binds sialic acid residues (neuraminic acid derivatives) on the host cell membrane → virus fusion with the membrane → entry into the cell
- The virus replicates in the nucleus of the cell.
- The new virus particles travel to the cell membrane → formation of a membrane bud around the virus particles (budding).
- Viral neuraminidase (N) cleaves the neuraminic acid → virions exit the cell.
- Host cell dies → cellular breakdown triggers a strong immune response
Clinical features
Complications
Secondary bacterial bronchitis and pneumonia
- Etiology: Common causative pathogens include S. pneumoniae, S. aureus (including MRSA), S. pyogenes, and H. influenzae.
- Pathophysiology
- Influenza virus attacks the tracheobronchial epithelium and results in decreased cell size and a loss of cilia, which promotes bacterial colonization.
- The influenza surface protein neuraminidase also cleaves sialic acid off host glycoproteins, leading to an increased amount of free sugar in the respiratory tract, which fosters bacterial growth.
- Clinical features
- Development of a purulent, productive cough ∼ 4–14 days after an initial period of improvement
- Recurrent fever
- Symptoms similar to community-acquired pneumonia
Diagnostics
Treatment
Prevention
Inactivated versions of the influenza vaccine stimulate the formation of neutralizing antibodies against the hemagglutinin antigen of included strains. Subsequent exposure to a strain of influenza included in the vaccine will not result in infection because the antibodies bind to hemagglutinin, thereby preventing hemagglutinin from attaching to the sialic acid receptor on host respiratory epithelial cells (preventing viral entry).