Staphylococcus epidermidis
-
Microbiology:
- Gram-positive cocci, typically in clusters.
- Catalase-positive.
- Coagulase-negative (differentiates from S. aureus).
- Urease-positive.
- Novobiocin-sensitive (differentiates from novobiocin-resistant S. saprophyticus).
-
Clinical Significance:
- Normal flora of the skin.
- Common cause of opportunistic infections, particularly in immunocompromised patients or those with indwelling medical devices.
- Key pathogen in infections of:
- Prosthetic devices: Artificial heart valves (prosthetic valve endocarditis - PVE), prosthetic joints, shunts (e.g., ventriculoperitoneal shunts).
- Intravascular catheters (central lines, IV catheters), leading to bacteremia and sepsis.
- Less commonly, native valve endocarditis.
- Frequently a contaminant of blood cultures due to its presence on the skin; clinical correlation is crucial.
-
Major Virulence Factor:
- Biofilm formation: Produces an extracellular polysaccharide slime layer (glycocalyx) that allows it to adhere strongly to foreign materials (plastics, metals) and protects it from host immune responses and antibiotics. This is critical for its pathogenesis on implanted devices.
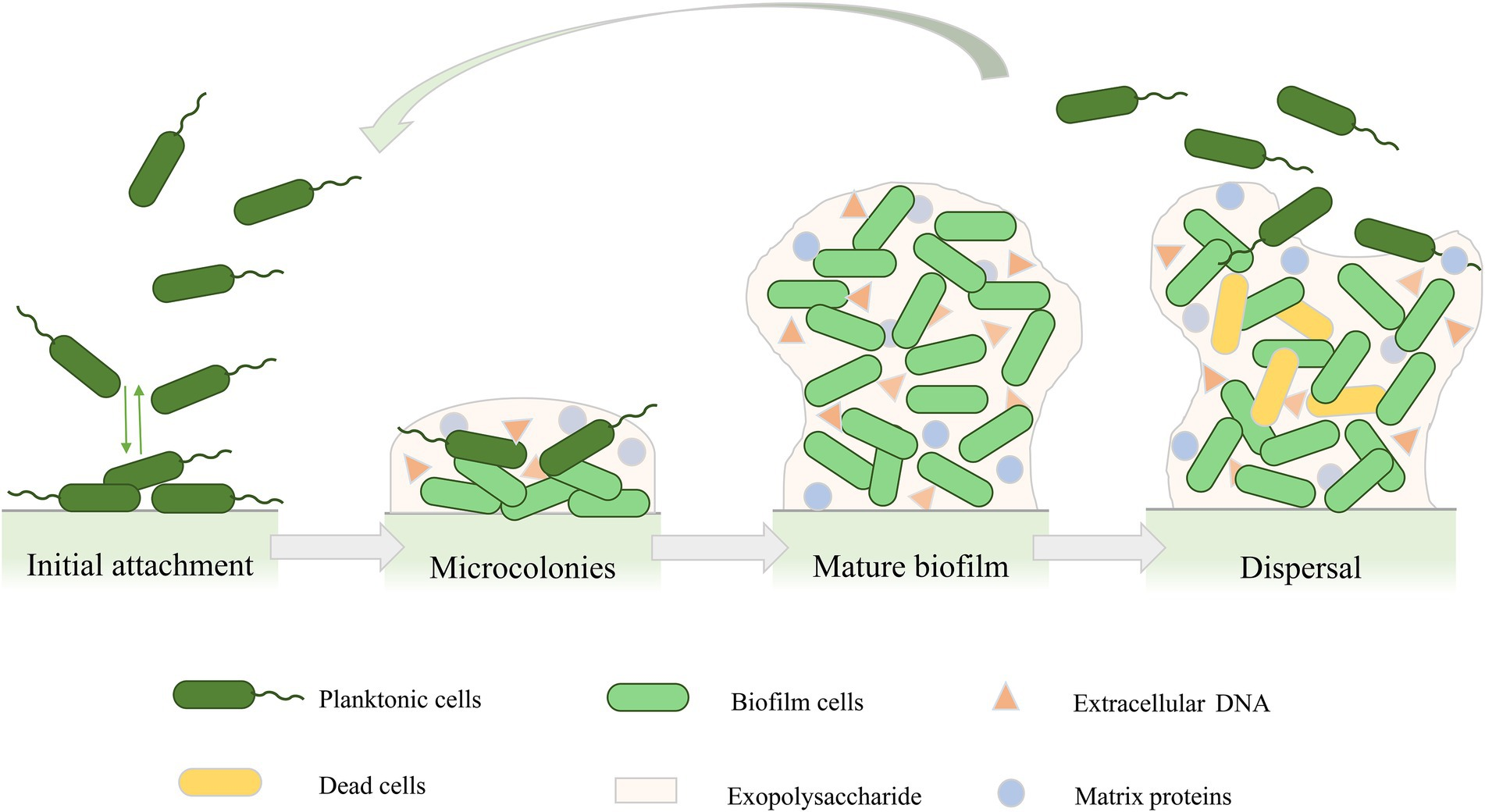
- Biofilm formation: Produces an extracellular polysaccharide slime layer (glycocalyx) that allows it to adhere strongly to foreign materials (plastics, metals) and protects it from host immune responses and antibiotics. This is critical for its pathogenesis on implanted devices.
-
Treatment:
- Often resistant to multiple antibiotics, including methicillin (Methicillin-Resistant S. epidermidis - MRSE).
- Vancomycin is typically the empiric drug of choice for serious infections.
- Management often requires removal of the infected foreign body/device in addition to antibiotic therapy.
- If susceptible, nafcillin or oxacillin can be used.