- Etiology
- Chronic Pancreatitis (most common cause; inflammation compresses the adjacent vein).
- Pancreatic carcinoma (distal/tail tumors).
- Abdominal trauma or surgery.
- Hypercoagulable states.
- Pathophysiology
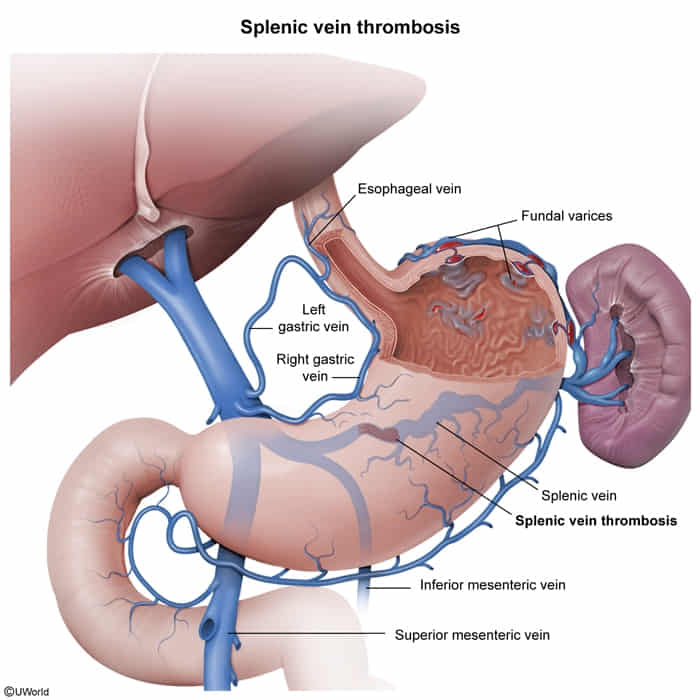
- Thrombosis of the splenic vein obstructs venous drainage from the spleen.
- Blood flow is redirected via collateral circulation: Spleen → Short gastric veins → Gastric fundus → Left gastric vein → Portal vein.
- Resulting high pressure in short gastric veins causes Isolated Gastric Varices (dilation of veins in the fundus). t
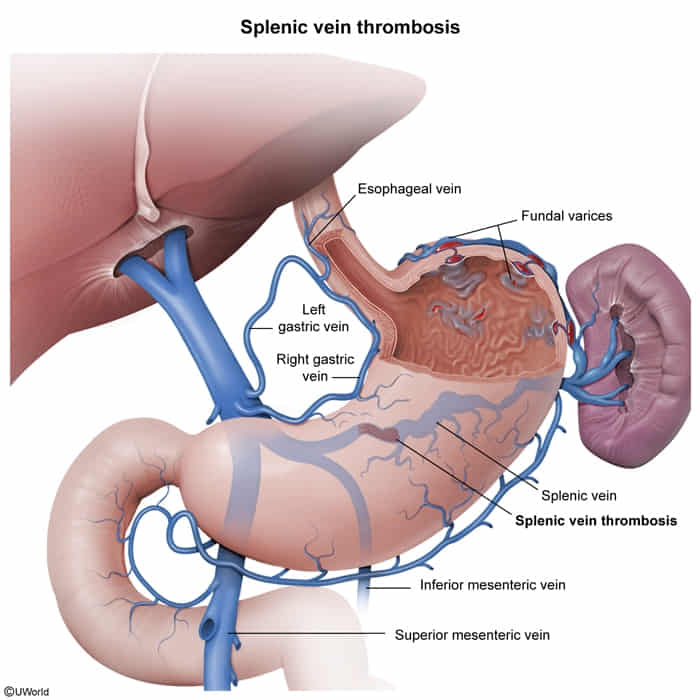
- Portal pressure remains normal (unless concurrent cirrhosis is present).
- Clinical Features
- Often asymptomatic until variceal rupture.
- Upper GI Bleeding: Hematemesis, melena.
- Splenomegaly (due to venous congestion).
- Hx of chronic alcohol use or pancreatitis.
- Key Distinction: Gastric varices ONLY (no esophageal varices).
- Diagnostics
- Abdominal CT with contrast: Venous phase shows thrombus in splenic vein and collateral vessels.
- Ultrasound: Visualization of thrombus; absence of flow.
- Endoscopy: Shows isolated varices in the gastric fundus; esophagus is usually normal.
- Treatment
- Splenectomy: Curative treatment for bleeding gastric varices due to SVT (eliminates the venous inflow to the collaterals).
- Observation: If asymptomatic (non-bleeding).
- Treat underlying cause (e.g., pancreatitis).