- Hemorrhagic necrotizing inflammation of the intestinal wall
- Most commonly affects the distal ileum and proximal colon
Epidemiology
NEC is the most common cause of acute abdomen in premature infants.
Etiology
- Patho/Etiology
- NEC is an acute inflammatory necrosis of the intestine, most commonly affecting the terminal ileum and colon.
- The pathogenesis is multifactorial, involving a combination of intestinal immaturity, gut ischemia, bacterial colonization of the gut, and enteral feeding.
- An exaggerated inflammatory response in the immature gut leads to bacterial invasion of the intestinal wall, inflammation, and necrosis.
- Risk Factors
- Prematurity: The single most significant risk factor; incidence is inversely proportional to gestational age.
- Low birth weight: Especially infants <1500g.
- Formula feeding: Breast milk is protective.
- Intestinal Ischemia: Can be caused by perinatal asphyxia, hypotension, or congenital heart disease.
Pathophysiology
Clinical features
- Typically occurs in the first few weeks of life, often after enteral feeds have been initiated.
- Early/Nonspecific signs: Lethargy, apnea, bradycardia, temperature instability, feeding intolerance (e.g., increased gastric residuals), and vomiting.
- Specific GI signs: Abdominal distension, tenderness, and bloody stools (hematochezia).
- Severe signs: Abdominal wall erythema (indicates peritonitis), palpable abdominal mass, shock.
Diagnostics
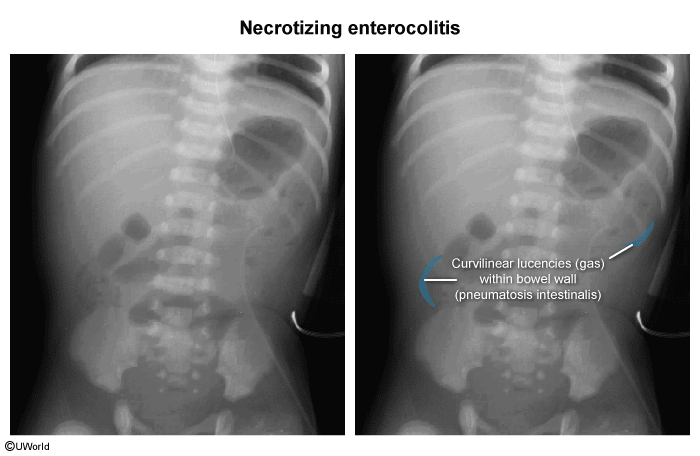
- Abdominal radiography
- Pneumatosis intestinalis: bubbles of gas within the wall of the intestine (“tram tracking”)
- Portal venous gas (pneumatosis hepatis)
- Increased intestinal wall thickness
- Pneumatosis intestinalis: bubbles of gas within the wall of the intestine (“tram tracking”)
Treatment
- Medical (for non-perforated NEC):
- Bowel Rest: Stop all enteral feeds (NPO).
- Gastric Decompression: Place an NG tube for suction.
- IV Fluids & TPN: Provide hydration and nutrition.
- Broad-spectrum IV antibiotics.
- Serial abdominal X-rays (e.g., every 6 hours) and physical exams to monitor for progression.
- Surgical:
- Absolute indication: Pneumoperitoneum (intestinal perforation).
- Other indications include clinical deterioration despite medical management or a fixed, dilated loop of bowel on serial X-rays.
- Procedure: Exploratory laparotomy with resection of necrotic bowel; an ostomy is often created.
- Prevention
- Antenatal Corticosteroids: Administering corticosteroids to mothers at risk for preterm delivery (<34 weeks) accelerates fetal lung and intestinal maturation, reducing NEC risk.
- Exclusive Human Milk Diet: Breast milk is highly protective and is a key preventative strategy. It contains immune factors (e.g., IgA), beneficial bacteria, and growth factors that promote gut health. Donor milk is a preferred alternative to formula if mother’s milk is unavailable.
- Probiotics: Supplementation with specific probiotic strains (e.g., Lactobacillus, Bifidobacterium) has been shown to reduce the risk of severe NEC and mortality, although specific protocols can vary.
- Standardized Feeding Protocols: Using slow, standardized protocols for advancing enteral feeds helps prevent overwhelming the immature gut.
Complications
- Short-term: Sepsis, peritonitis, shock, and death (mortality can be up to 50%).
- Long-term:
- Intestinal strictures (can occur in up to 39% of infants), leading to obstruction.
- Short bowel syndrome if significant bowel resection is required, leading to malabsorption and dependence on TPN.
- Neurodevelopmental delay.