Intestinal ischemia
Colon ischemia (Ischemic colitis)
-
Pathophysiology/Etiology
- Reduced blood flow to the colon, leading to inflammation and injury. Most cases are due to non-occlusive ischemia (e.g., "low-flow" state like shock, heart failure, sepsis) rather than acute arterial occlusion.
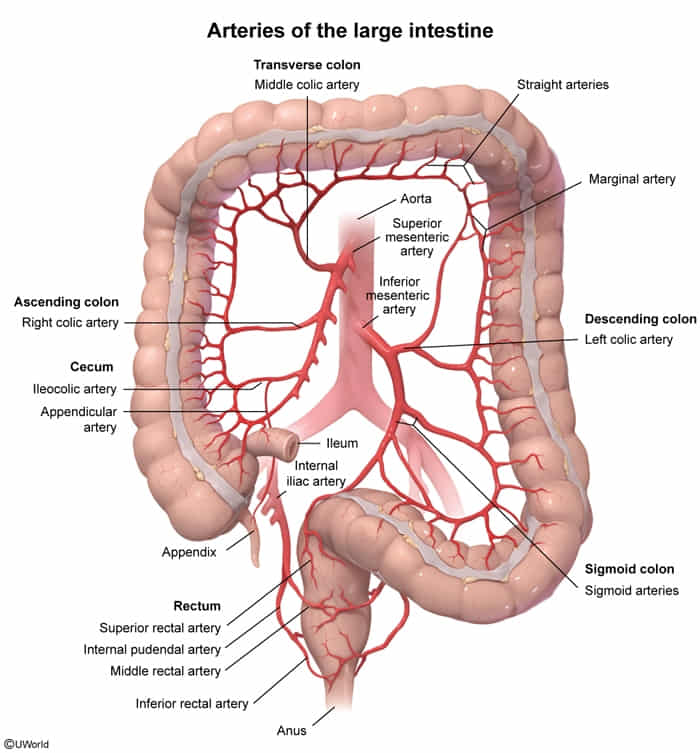
- Watershed areas are most vulnerable due to limited collateral blood supply.
- Splenic flexure (Griffith's point): junction of SMA and IMA territories.
- Rectosigmoid junction (Sudeck's point): junction of IMA and iliac artery territories.
- Risk factors: elderly age (>60), atherosclerosis, hypotension, heart failure, aortic surgery (esp. AAA repair with IMA ligation), vasculitis, hypercoagulable states.
-
Clinical Presentation
- Classic triad: rapid onset of mild-to-moderate crampy abdominal pain (often left-sided), followed by hematochezia (bright red blood per rectum) or bloody diarrhea within 24 hours.
- Nausea, vomiting, and diarrhea may also occur.
- Peritoneal signs (rigidity, guarding) suggest transmural necrosis and perforation (a surgical emergency).
-
Diagnosis
- CT scan with IV contrast is the best initial imaging test to rule out other causes of abdominal pain and support the diagnosis.
- Findings: segmental bowel wall thickening ("thumbprinting"), submucosal edema, and pericolonic fat stranding.
- Severe findings: pneumatosis (gas in the bowel wall) or portal venous gas indicate infarction.
- Colonoscopy is the gold standard for diagnosis, showing edematous, friable mucosa, petechial hemorrhages, and segmental erythema. It should be performed without aggressive insufflation to avoid perforation.
- Labs are nonspecific but may show leukocytosis and elevated lactate in severe cases.
- CT scan with IV contrast is the best initial imaging test to rule out other causes of abdominal pain and support the diagnosis.
-
DDx (Differential Diagnosis)
- Infectious colitis (e.g., C. difficile, E. coli O157:H7, Campylobacter): Differentiated by stool cultures and specific toxin assays. Often has more profuse watery diarrhea and fever.
- Inflammatory Bowel Disease (IBD) (Ulcerative Colitis/Crohn's): Onset is typically more gradual and chronic. Biopsy is key. UC pain is often LLQ, while Crohn's is often RLQ.
- Diverticulitis: Presents with LLQ pain and fever but usually without significant bleeding.
- Acute mesenteric ischemia (AMI): Much more severe "pain out of proportion to exam," often caused by an embolism to the SMA. Involves the small bowel. Requires angiography for diagnosis.
-
Management/Treatment
- Most cases are transient and resolve with supportive care.
- Bowel rest (NPO), IV fluids to restore perfusion, and correction of underlying causes.
- Broad-spectrum antibiotics (e.g., piperacillin-tazobactam or a fluoroquinolone plus metronidazole) are given to prevent bacterial translocation and sepsis.
- Surgical intervention (colectomy) is required for patients with signs of peritonitis, bowel gangrene, or perforation.
-
Key Associations/Complications
- Complications: Gangrene, perforation, hemorrhage, and post-ischemic stricture formation.
- Prognosis: Most patients recover fully with medical management. However, mortality is high if surgery is needed. Isolated right-sided colonic ischemia has a worse prognosis.