Epidemiology
Etiology
Pathophysiology
Replication cycle of HBV
HBV carries a DNA polymerase with both DNA and RNA-dependent functions, also known as reverse transcriptase (RT).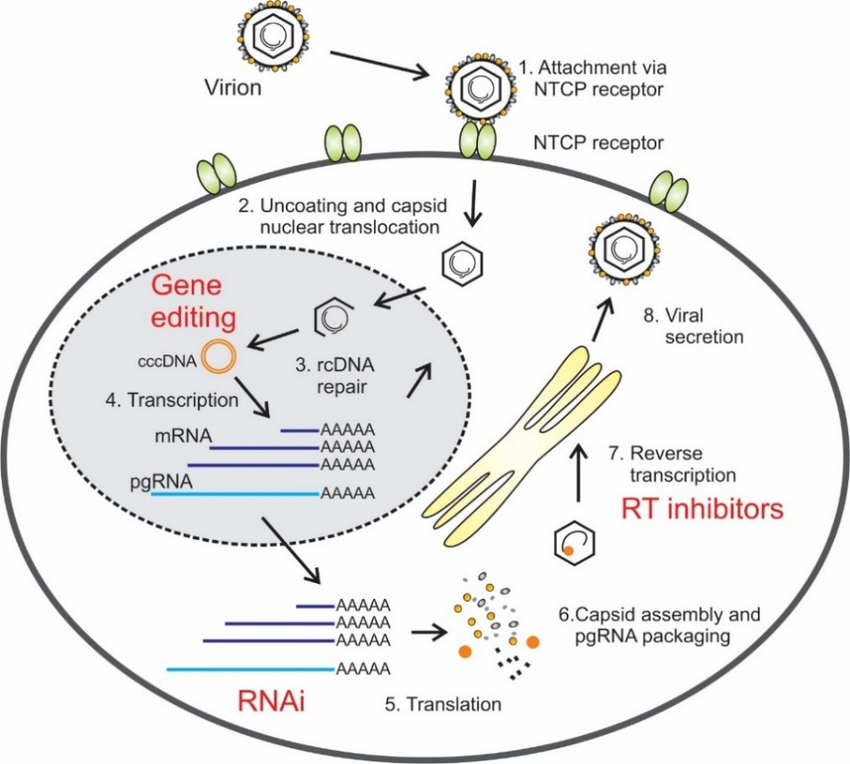
-
Entry: Virus enters the hepatocyte and the nucleocapsid travels to the nucleus.
-
cccDNA Formation: Inside the nucleus, the viral partially double-stranded DNA (rcDNA) is “repaired” by host enzymes into a stable covalently closed circular DNA (cccDNA).
- Key Point: cccDNA acts as a persistent template for all viral transcription, leading to chronic infection.
-
Transcription: Host RNA polymerase transcribes the cccDNA into messenger RNAs (mRNAs) and a key pregenomic RNA (pgRNA) intermediate.
-
Assembly & Reverse Transcription: In the cytoplasm, viral proteins, polymerase, and the pgRNA are packaged into a new core particle.
- Key Point: The HBV polymerase acts as a reverse transcriptase, using the pgRNA template to synthesize the new rcDNA genome.
- HBV polymerase has both RNA- and DNA-dependent DNA polymerase activity
-
Release: New virions acquire an envelope with HBsAg and are secreted from the cell.
Clinical features
Outcomes
- Acute hepatitis with complete resolution
- Most common, > 95% in infected adults
- Chronic hepatitis (with or without cirrhosis and the attendant increased risk of hepatocellular carcinoma)
- Fulminant hepatitis with massive liver necrosis.
Diagnostics
Tip
- HBsAg: infection or not
- Anti-HBc: acute (IgM) or chronic (IgG); current & history infection vs immunized (The HBV vaccine contains only one viral protein: HBsAg)
- Anti-HBs
- Meaning: Immunity.
- Indicates recovery from natural infection OR response to vaccination.
Tip
Markers that can’t coexist:
- HBsAg & Anti-HBs
- HBeAg & Anti-HBe
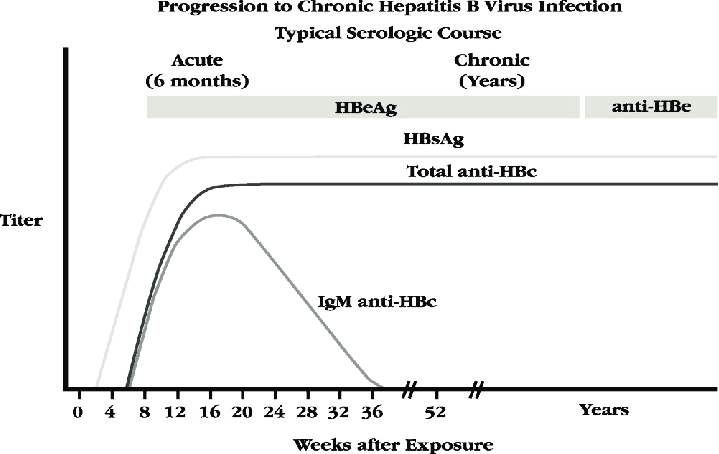
- The “Window Period”: The time gap between the disappearance of HBsAg and the appearance of Anti-HBs.
- Both surface markers are negative.
- Diagnosis relies on IgM Anti-HBc or HBV DNA.
- Chronic infection (inactive): HBsAg (+), Anti-HBc (+, IgG), Anti-HBe (+)
- Recovery: conversion from HBsAg (+) to Anti-Hbs (+) in chronic infection, also HBV DNA needs to be undetectable
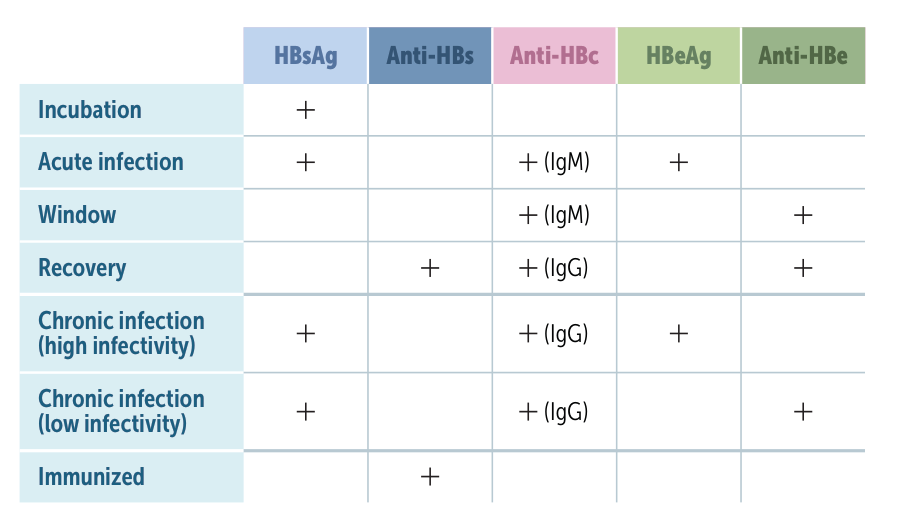
- Vaccinated vs. Recovered:
- Vaccinated: Anti-HBs (+) only. (Received the surface antigen spike only).
- Recovered: Anti-HBs (+) AND Anti-HBc (+). (Immune system saw the “core” of the virus during actual infection). t
Window period
During the window period, anti-HBc IgM and anti-HBe may be positive. But they don’t give a clear picture of current infectiousness because they may indicate previous infection.
Pathology
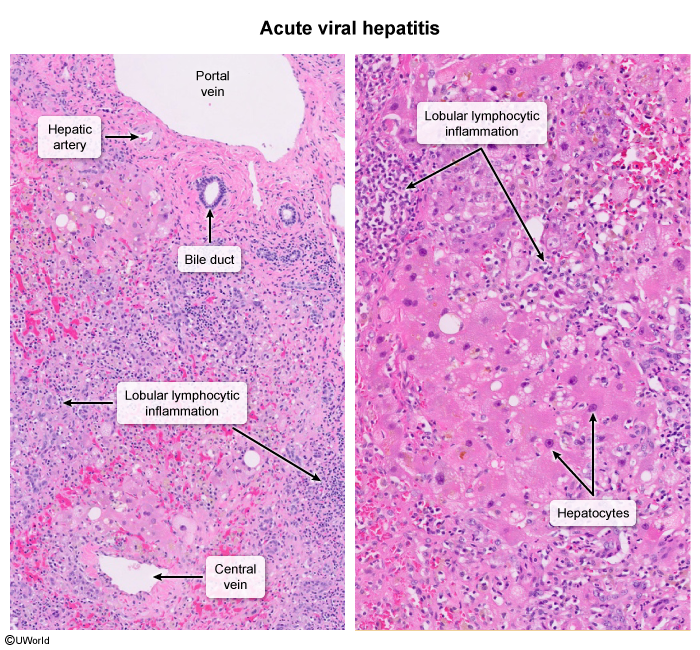
Active viral hepatitis
Tip
Most cases are marked by significant panlobular lymphocytic inflammation (ie, involving the entire lobule), which develops in response to the viral antigens. To control the infection, cytotoxic T cells trigger apoptosis of infected hepatocytes by binding death receptors (eg, Fas) on the plasma membrane and by secreting cytotoxic mediators (eg, perforins, granzymes). As a result, a cascade of caspase enzymes breaks down hepatocyte proteins and DNA, leading to cell shrinkage, chromatin condensation and fragmentation, and budding apoptotic bodies (ie, membrane-bound cellular fragments).
- Eosinophilic single-cell necrosis (Councilman bodies) t
- An eosinophilic remnant of apoptotic hepatocytes seen on liver biopsy. Associated with yellow fever and viral hepatitis.
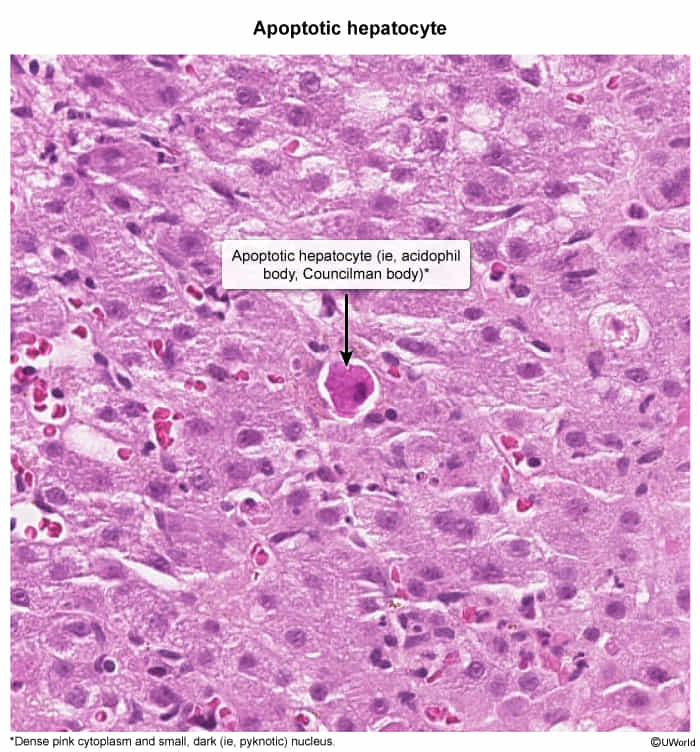
- An eosinophilic remnant of apoptotic hepatocytes seen on liver biopsy. Associated with yellow fever and viral hepatitis.
- Bridging necrosis
Chronic viral hepatitis
- Interface hepatitis (piecemeal necrosis)
- Periportal liver cell necrosis with lymphocytic infiltration
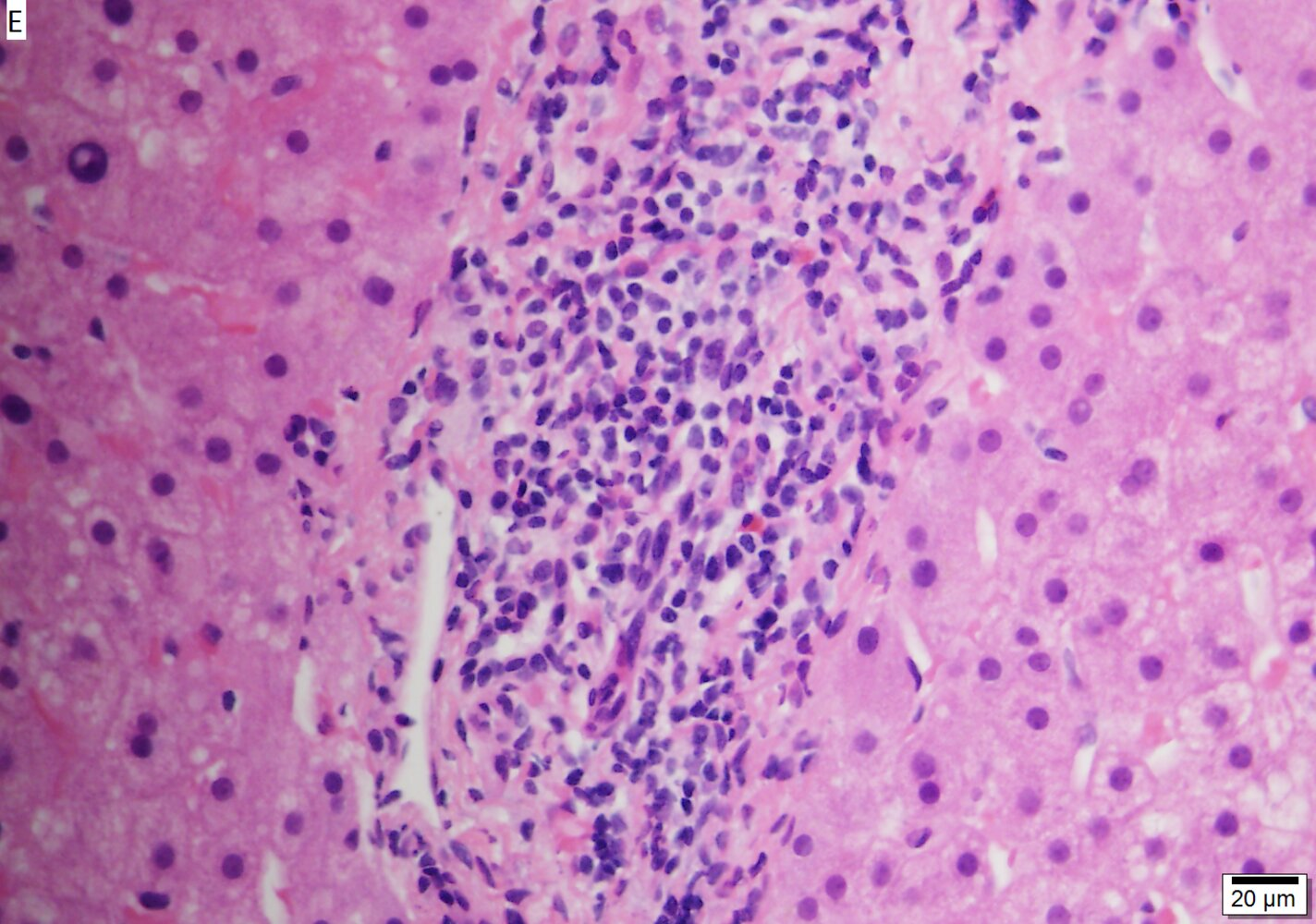
- The cause of interface hepatitis is a CD8 T-cell‑induced hepatocyte apoptosis.
- Indicates chronic active hepatitis and poor prognosis
- Periportal liver cell necrosis with lymphocytic infiltration
- Fibrous septa
- Ground glass hepatocytes (Characteristic for HBV)
- Accumulation of hepatitis B surface antigen within infected hepatocytes. This results in the appearance of a finely granular, homogeneous, pale eosinophilic cytoplasm (ground-glass hepatocytes).
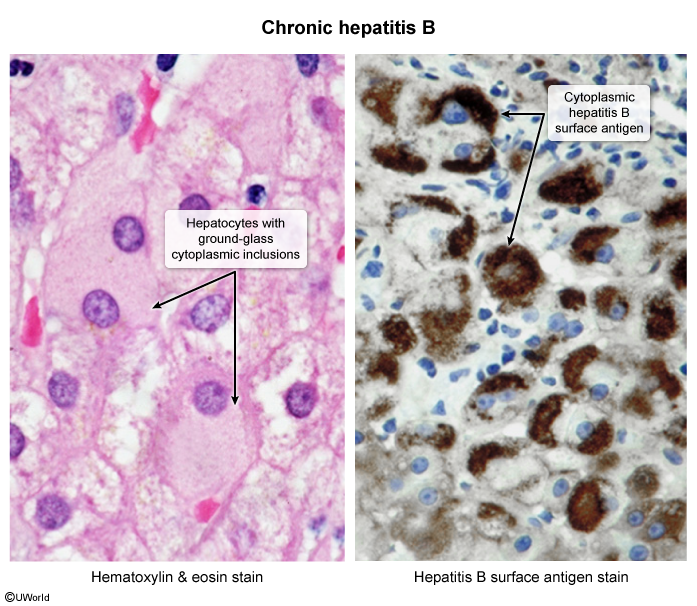
- Pathognomonic for hepatitis B
- Accumulation of hepatitis B surface antigen within infected hepatocytes. This results in the appearance of a finely granular, homogeneous, pale eosinophilic cytoplasm (ground-glass hepatocytes).
Treatment
- Goal: Suppress HBV DNA, normalize ALT, prevent cirrhosis & HCC.
- Who to Treat:
- High HBV DNA + High ALT (>2x ULN).
- All patients with cirrhosis, regardless of labs.
- First-Line Drugs (Oral Nucleos(t)ide Analogs - NAs):
- High barrier to resistance; long-term/lifelong therapy.
- Tenofovir (TDF or TAF): Preferred agents. TDF: Risk of nephrotoxicity & ↓ bone density. TAF: Safer for kidneys and bones.
- Entecavir (ETV): Also a potent first-line choice.
- Alternative (Injectable):
- Pegylated Interferon alfa-2a (PEG-IFN): Finite therapy course (48 wks). Higher chance of HBsAg clearance. Major side effects: Flu-like Sx, depression, cytopenias. Contraindicated in decompensated cirrhosis.
- Key Scenarios:
- Pregnancy: If viral load is high (>200,000 IU/mL), treat with TDF starting in the 3rd trimester to prevent vertical transmission.
- Newborn Prophylaxis: HBV vaccine + HBIG at birth.
- HIV Coinfection: HIV regimen must include Tenofovir + (Lamivudine or Emtricitabine).
Prevention
Perinatal Hep B
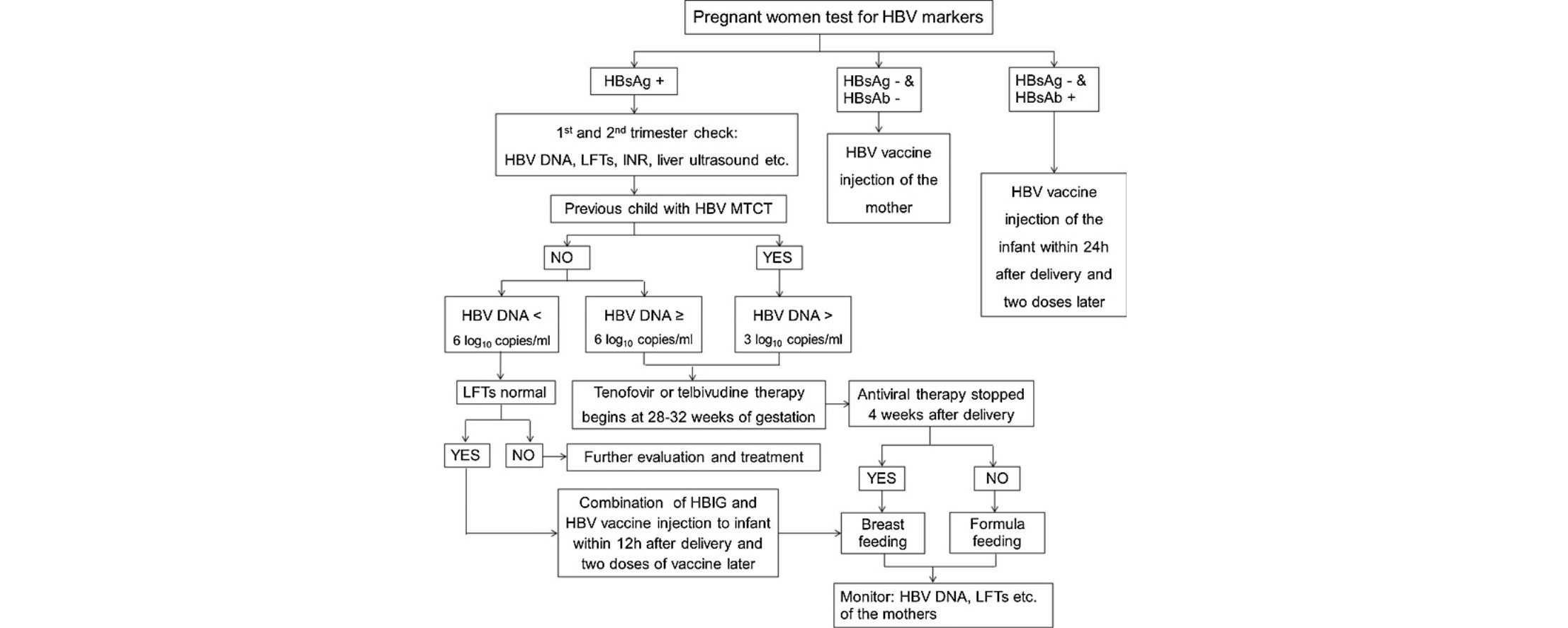
- Breastfeeding may be started immediately if there are no contraindications (e.g., cracked or bleeding nipples), regardless of whether individuals:
- Have HBsAg positive or unknown status
- Are receiving antiviral therapy
- Infants with HBV infection
- Infants usually immune-tolerant (normal or mildly elevated liver enzymes, no symptoms)
- Because HBV is not cytopathic itself and newborns lack mature cytotoxic T-cells that mediate damage infected hepatocytes, the degree of hepatic tissue damage will be very limited.
- High risk for chronic infection
- High viral load & HBeAg positive
- Infants usually immune-tolerant (normal or mildly elevated liver enzymes, no symptoms)
Hepatitis D
- Pathogen: hepatitis D virus (HDV)
- Comprises an outer lipoprotein envelope made of the hepatitis B surface antigen (HBsAg) for entry into host cells and an inner ribonucleoprotein structure in which the HDV genome resides
- Epidemiology: 5% of all patients with chronic HBV infection carry HDV.