Etiology
- Genetic factors
- Medullary carcinoma: associated with MEN2 (RET gene mutations) or familial medullary carcinoma
- Papillary carcinoma: associated with RET/PTC rearrangements and BRAF mutations
- Follicular carcinoma: associated with PAX8-PPAR-γ rearrangement and RAS mutation
- Undifferentiated/anaplastic carcinoma: associated with TP53 mutation
- Ionizing radiation (particularly during childhood): mostly associated with papillary carcinoma
Overview
| Feature | Papillary (PTC) | Follicular (FTC) | Medullary (MTC) |
|---|---|---|---|
| Origin | Follicular Cells | Follicular Cells | Parafollicular C-Cells |
| Key Histo | - Orphan Annie eye nuclei - Psammoma bodies | - Capsular/Vascular invasion | - Amyloid deposits (Congo red) |
| Spread | Lymphatic | Hematogenous (blood) | Both Lymphatic & Hematogenous |
| Marker/Gene | - BRAF, RET/PTC - Prior Radiation | - RAS - Iodine deficiency | - Calcitonin (tumor marker) - RET mutation (MEN 2A/2B) |
| Prognosis | Excellent | Good | Fair (worse than PTC/FTC) |
Tip
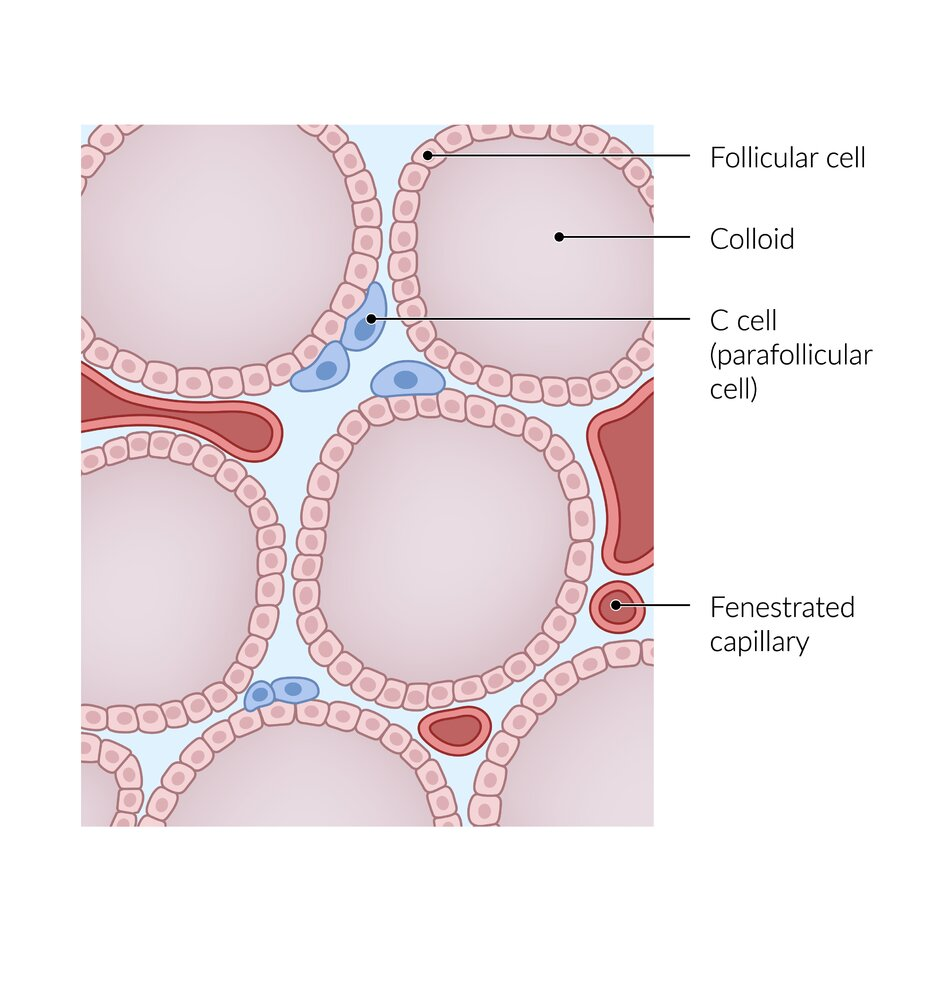
- Papillary Thyroid Carcinoma (PTC): Originates from the follicular cells of the thyroid gland. These cells are responsible for producing thyroid hormones. PTC is the most common type of thyroid cancer.
- Follicular Thyroid Carcinoma (FTC): Also originates from the follicular cells of the thyroid gland. Follicular and Papillary carcinoma are differentiated thyroid cancers.
- Medullary Thyroid Carcinoma (MTC): Arises from the parafollicular cells (also known as C cells) of the thyroid gland. These cells are distinct from follicular cells, and they produce the hormone calcitonin, which is involved in calcium regulation. MTC is a neuroendocrine tumor.
Papillary thyroid carcinoma
- Tissue of origin: Thyrocytes
- Well differentiated
- Characteristics
- Most common type of thyroid cancer
- Palpable lymph nodes due to metastatic spread (often detected before primary tumor)
- May be multifocal
- Very good prognosis
- Pathology
- Psammoma bodies
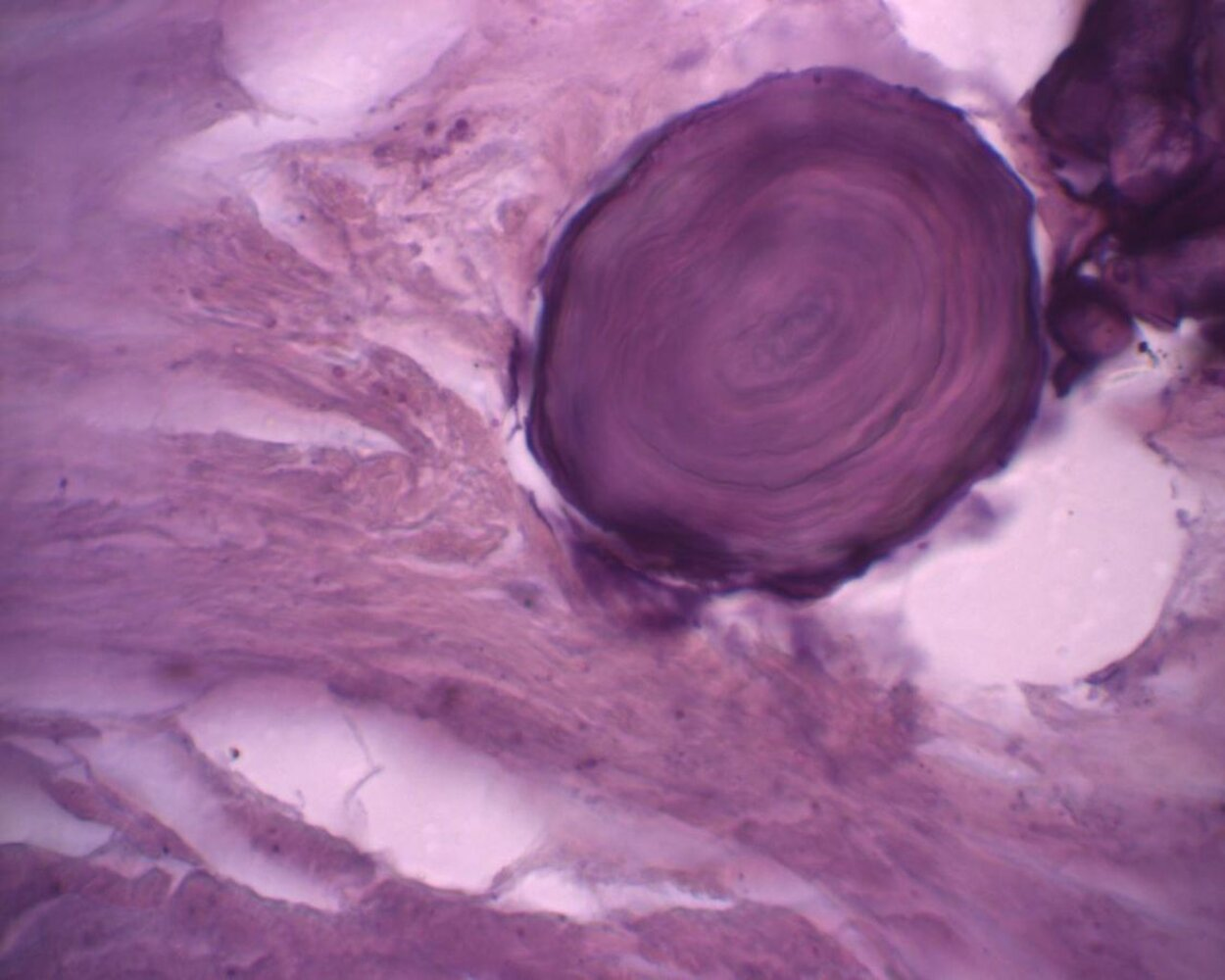
- Morphology: concentric lamellar calcifications
- Occurrence: seen in diseases associated with calcific degeneration
- Papillary thyroid carcinomas (evidence of psammoma bodies in thyroid tissue should always raise suspicion of malignancy)
- Serous papillary cystadenocarcinoma of ovary and endometrium
- Meningiomas
- Mesotheliomas
- Intranuclear inclusions (pseudoinclusions): These are not true inclusions of chromatin within the cytoplasm. They are actually invaginations (infoldings) of the nuclear membrane (the envelope that surrounds the nucleus). Because of this infolding, cytoplasm appears to be inside the nucleus, but it’s actually still separated from the nuclear material by the folded nuclear membrane.
- Nuclear grooves: These are also invaginations of the nuclear envelope, creating a groove or fold in the nucleus. It gives a characteristic appearance sometimes likened to a “coffee bean”.
- “Orphan Annie” eyes nuclei
- Morphology: empty-appearing large oval nuclei with central clearing
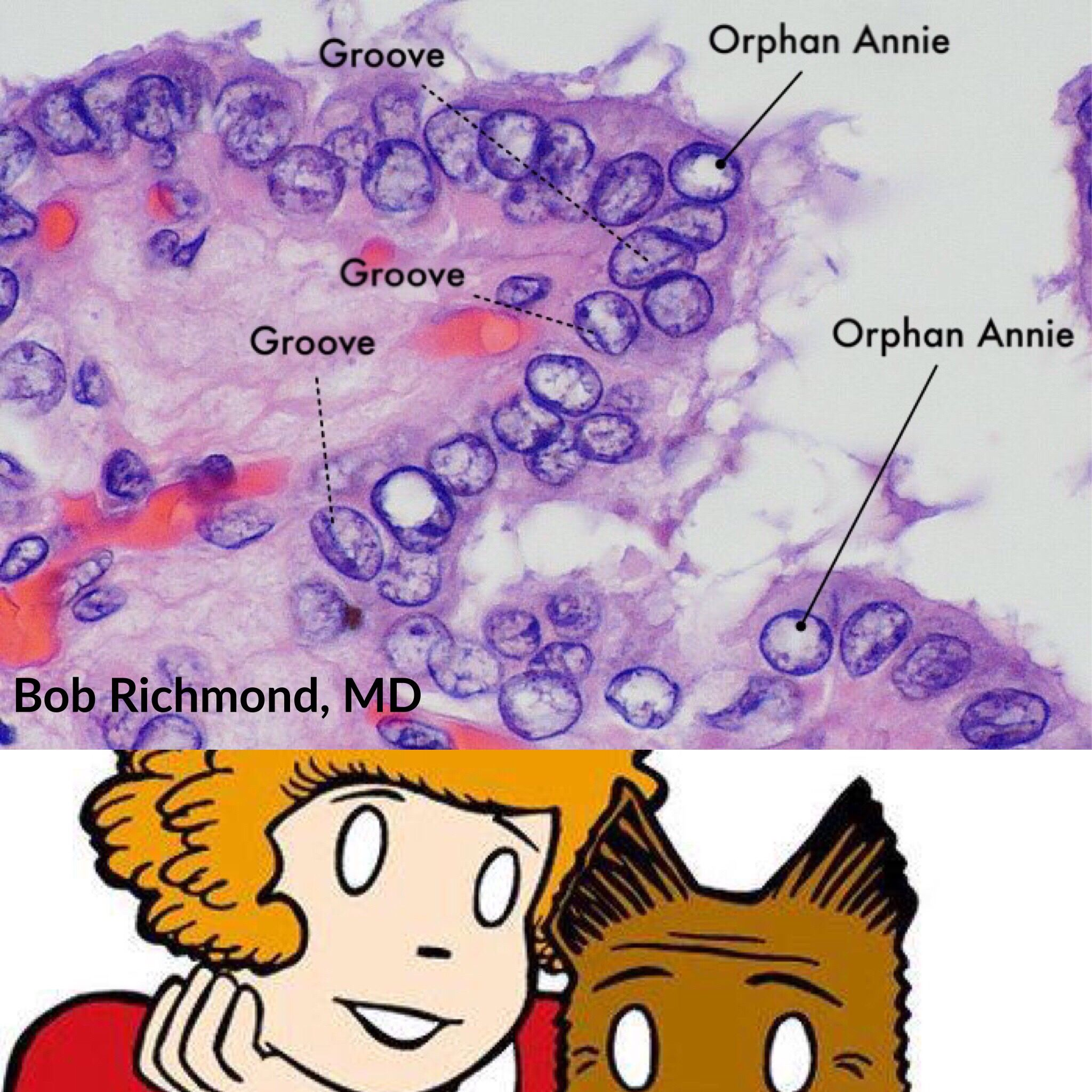
- Occurrence
- Papillary thyroid carcinomas
- Autoimmune thyroiditis (e.g., Hashimoto disease, Grave disease)
- Morphology: empty-appearing large oval nuclei with central clearing
- Psammoma bodies
Mnemonic
Papi and Moma adopted Orphan Annie.
Follicular thyroid carcinoma
- Well differentiated
- Characteristics
- Hematogenous metastasis especially to
- Lungs
- Bone (lytic lesions)
- Rarely multifocal
- Distinguishing a benign follicular adenoma from a well-differentiated follicular carcinoma depends on the presence of vascular or capsular invasion, which cannot be determined on a fine-needle aspiration specimen.
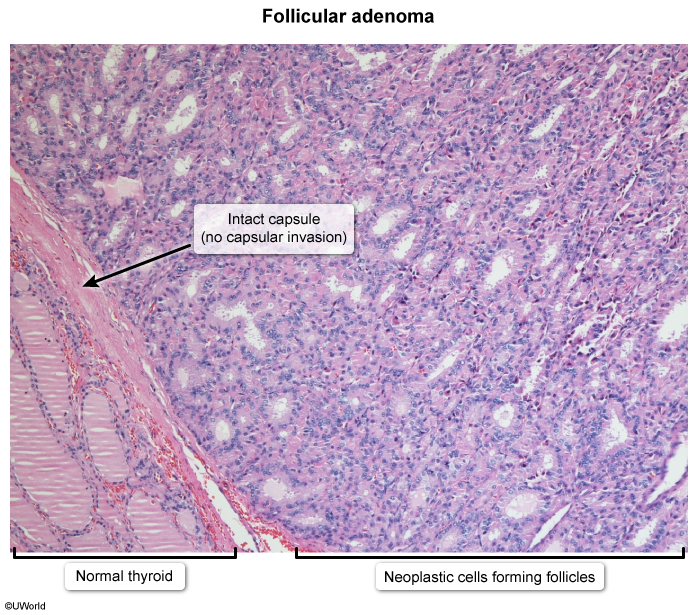
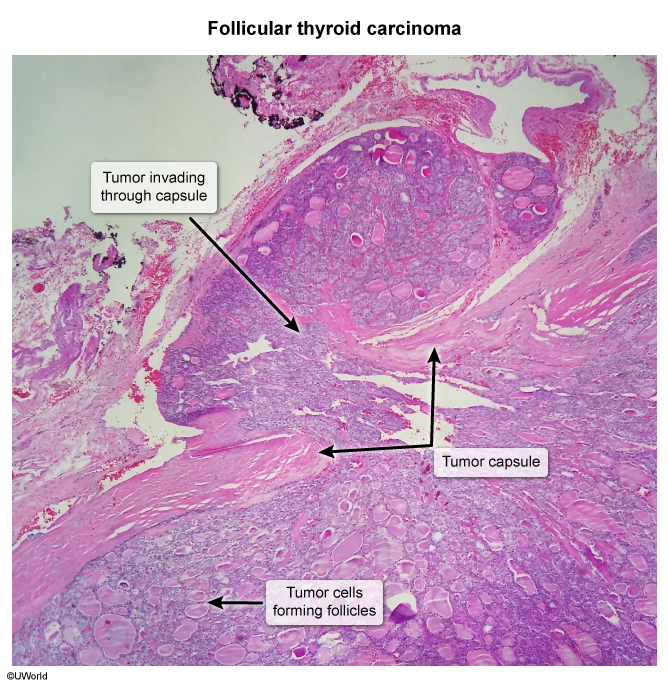
- Good prognosis
- Hematogenous metastasis especially to
Medullary carcinoma
- Tissue of origin: Parafollicular cells (C cells)
- The parafollicular cells are located in the connective tissue between the thyroid follicles, which can be considered a “medullary” (central) part of the thyroid gland, although not in the same sense as the medulla in other organs like the adrenal glands.
- Poorly differentiated
- Characteristics
- Sometimes a genetic predisposition → multiple endocrine neoplasia type 2 (MEN2) (25% of medullary carcinomas)
- Sporadic (75% of medullary carcinomas)
- Produces calcitonin
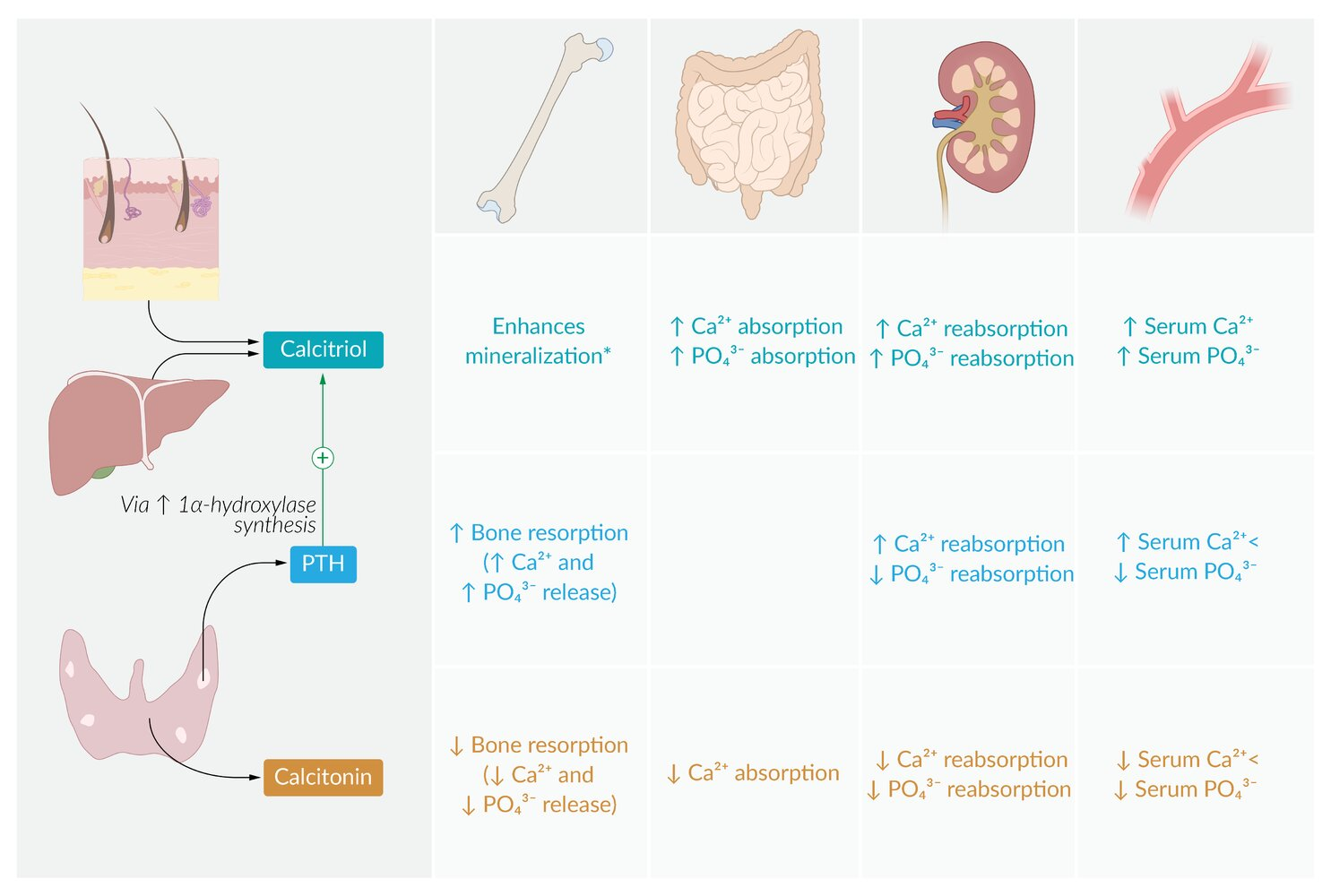
- Pathology
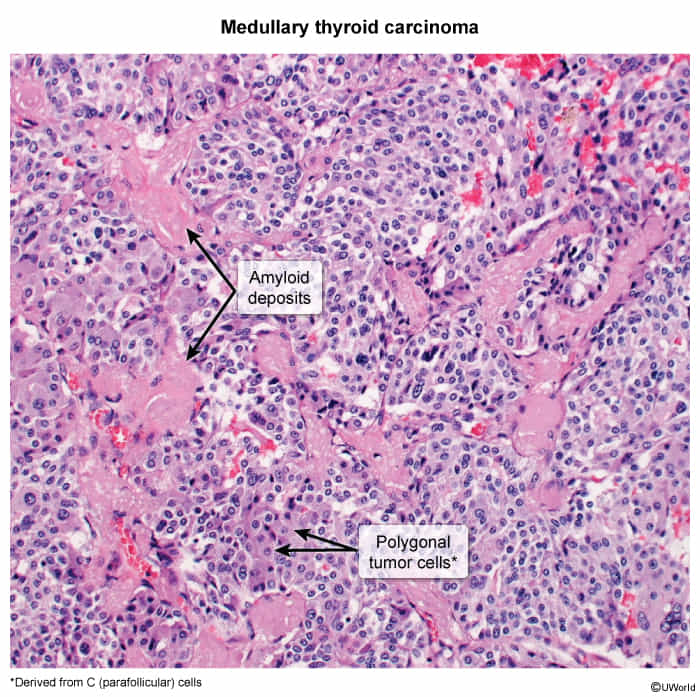
- Ovoid cells of C cell origin and therefore without follicle development
- Amyloid in the stroma (stains with Congo red)
- These amyloid deposits are derived from calcitonin secreted by the neoplastic C cells
Treatment
Thyroid surgery
Complications
- Transient/permanent postoperative hypoparathyroidism (most common) or hypothyroidism
- Hematoma
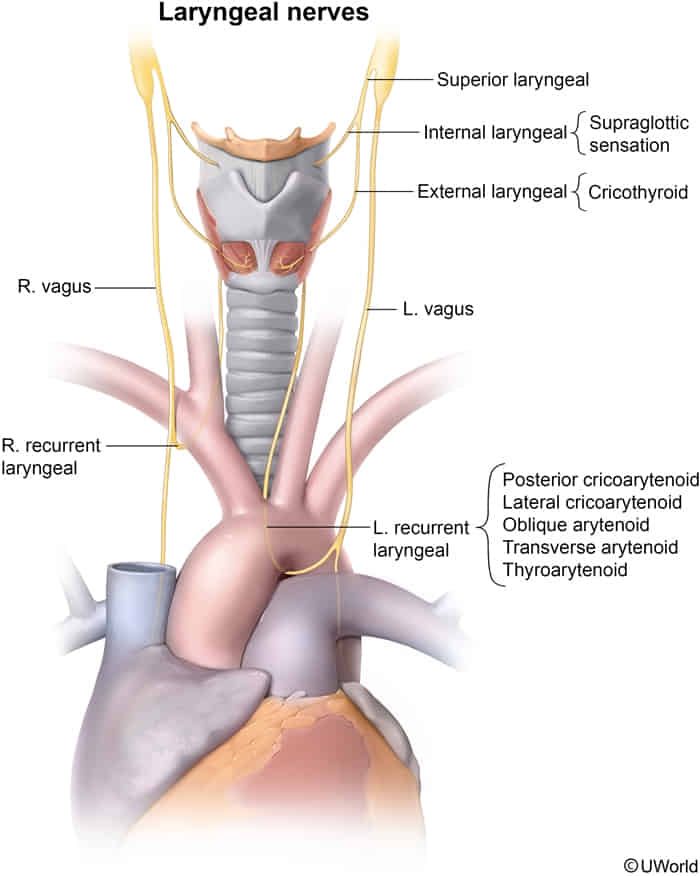
- Transient/permanent recurrent laryngeal nerve palsy (controls all laryngeal muscles except cricothyroid muscle)
- Unilateral RLN palsy
- Husky/hoarse voice
- Ineffective cough
- Risk of aspiration pneumonia
- Bilateral RLN palsy
- Unilateral RLN palsy
- Superior laryngeal nerve palsy → paralysis of cricothyroid muscle → easy voice fatigability; change in the timbre of voice