Pharmacodynamics
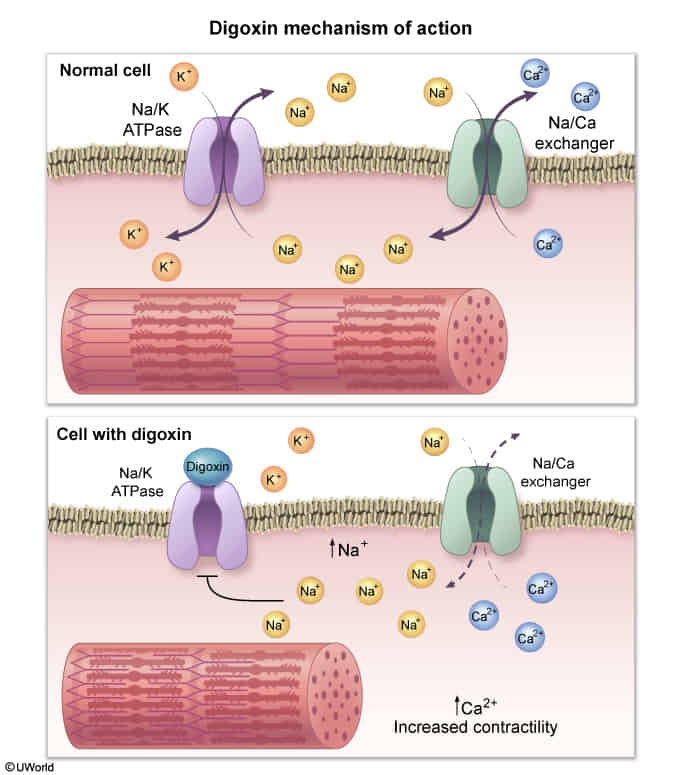
- Direct inhibition of the Na+/K+ ATPase in cardiac myocytes.
- This leads to ↑ intracellular Na+, which reduces the activity of the Na+/Ca2+ exchanger.
- The result is ↑ intracellular Ca2+, leading to increased contractility (positive inotropy).
- Also increases vagal tone, which slows conduction through the AV node and decreases heart rate.
Digoxin poisoning
Risk factors
- Renal Insufficiency: Decreases clearance.
- Hypokalemia: Usually from concurrent Loop Diuretic use (Lasix). Low K+ allows Digoxin to bind more avidly to the Na+/K+ ATPase pump. c
- Drugs that increase digoxin levels by decreasing clearance or displacing it from tissue binding sites (e.g., Amiodarone, Verapamil, Quinidine, Spironolactone).
Tip
- Hypokalemia precipitates toxicity (makes patient sensitive to the drug).
- Hyperkalemia is a result of acute toxicity (pump inhibition prevents K+ from entering cells) and is a marker for mortality.
Clinical features
- Gastrointestinal (Earliest/Most Common): Nausea, vomiting, anorexia, abdominal pain.
- Neurologic/Visual: Confusion, weakness, Xanthopsia (yellow-green vision), halos around lights.
- Cardiac: Palpitations, syncope, dyspnea.
ECG Findings
- Digoxin Effect (Therapeutic level, not toxicity):
- Scooped ST segment depressions (“Salvador Dalí moustache” or “reverse tick” sign).
- T-wave flattening or inversion.
- Shortened QT interval.
- Toxic ECG Changes:
- Most common: Frequent premature ventricular contractions (PVCs).
- Most Specific: Atrial Tachycardia with AV Block (due to increased automaticity + increased vagal tone). c
Diagnosis
- The diagnosis is primarily clinical, based on symptoms and ECG findings.
- Serum digoxin levels can be helpful but do not always correlate with toxicity, especially in chronic cases where electrolyte disturbances can cause toxicity even within the “therapeutic” range (0.5-2.0 ng/mL).
- Hyperkalemia is the most significant prognostic indicator in acute poisoning.
Management
- Supportive Care: Stop digoxin, correct electrolyte abnormalities (especially K+ and Mg2+), and provide continuous cardiac monitoring.
- Atropine: For severe bradycardia.
- Activated Charcoal: May be used for acute ingestion if within 1-2 hours.
- Antidote: Digoxin-specific antibody fragments (DigiFab/Digibind).
- Indications: Life-threatening arrhythmias (e.g., ventricular tachycardia, severe bradycardia), K+ >5.5 mEq/L in an acute setting, or end-organ dysfunction from hypoperfusion.
- After Fab fragments are given, serum digoxin levels are unreliable as they measure both bound and free drug.